County Health Rankings offer a compelling lens through which to examine the health of communities across the nation. This initiative provides a snapshot of health outcomes, identifying strengths and weaknesses within counties and highlighting disparities in health status. By analyzing key health indicators, the rankings shed light on factors influencing overall well-being, from socioeconomic conditions to environmental factors and healthcare access.
The rankings go beyond simply presenting numbers; they provide a framework for understanding the complex interplay of factors that contribute to health disparities. They serve as a powerful tool for policymakers, public health professionals, and community members to identify areas for improvement and develop targeted interventions to enhance health equity.
Overview of County Health Rankings
The County Health Rankings are an annual assessment of the health of nearly every county in the United States. They provide a comprehensive snapshot of the health status of communities across the country, highlighting both areas of strength and areas needing improvement.The rankings are a valuable resource for policymakers, community leaders, and individuals seeking to understand the factors that influence health outcomes in their communities.
By providing a clear picture of health disparities and trends, the rankings can help to inform and guide efforts to improve health and well-being at the local level.
Methodology for Compiling the Rankings
The County Health Rankings use a data-driven approach to assess health outcomes and factors that influence health. The methodology involves analyzing a wide range of data sources, including:
- Health Outcomes:The rankings consider two key health outcomes: length of life (measured by premature death rates) and quality of life (measured by the rate of poor physical and mental health days).
- Factors Influencing Health:The rankings analyze a broad set of factors that contribute to health outcomes, including:
- Health Behaviors:This category includes factors such as smoking rates, obesity rates, and physical inactivity levels.
- Clinical Care:This category assesses access to and quality of healthcare services, including preventive care, primary care, and specialty care.
- Social and Economic Factors:This category includes factors such as poverty rates, education levels, unemployment rates, and access to healthy foods.
- Physical Environment:This category considers factors such as air and water quality, access to parks and green spaces, and rates of violent crime.
The rankings are compiled using a standardized methodology that allows for comparisons across counties, regardless of their size, location, or population characteristics. This approach provides a consistent framework for understanding health disparities and identifying areas where interventions can be most effective.
Key Health Indicators
The County Health Rankings use a set of key health indicators to measure the overall health of communities across the United States. These indicators are grouped into four main categories: health factors, health outcomes, social determinants of health, and policy factors.
The rankings consider a variety of factors that contribute to health, encompassing both individual choices and community-level influences. The selection of these indicators is based on their proven association with health outcomes, their ability to be measured reliably, and their relevance to public health priorities.
Health Factors
Health factors are behaviors and conditions that influence health. They represent the things people can do to improve their health.
- Health Behaviors: These include behaviors that individuals can control, such as smoking, physical activity, and diet.
- Smoking rates: This metric measures the percentage of adults who smoke cigarettes.
- Obesity rates: This metric measures the percentage of adults who are obese.
- Physical inactivity rates: This metric measures the percentage of adults who do not engage in regular physical activity.
- Excessive drinking rates: This metric measures the percentage of adults who engage in excessive alcohol consumption.
- Clinical Care: This category includes access to and quality of healthcare services.
- Uninsured rates: This metric measures the percentage of people who lack health insurance.
- Preventable hospitalizations: This metric measures the number of hospitalizations that could have been prevented through better access to healthcare.
- Access to primary care: This metric measures the availability of primary care providers in a community.
- Social and Economic Factors: This category includes factors that influence health but are not directly related to healthcare.
- High school graduation rates: This metric measures the percentage of adults who have completed high school.
- Unemployment rates: This metric measures the percentage of adults who are unemployed.
- Income inequality: This metric measures the gap between the richest and poorest members of a community.
- Physical Environment: This category includes factors related to the physical environment, such as air and water quality.
- Air pollution: This metric measures the level of air pollutants in a community.
- Drinking water quality: This metric measures the quality of drinking water in a community.
County health rankings provide valuable insights into the well-being of communities across the nation. These rankings often highlight areas where improvements can be made, and organizations like Cigna play a crucial role in addressing these challenges. If you’re passionate about improving health outcomes, consider exploring Cigna health care careers , where you can contribute to a healthier future.
By working together, we can create a positive impact on county health rankings and build healthier communities for everyone.
- Access to parks and recreation: This metric measures the availability of parks and recreation facilities in a community.
Health Outcomes
Health outcomes are the results of the health factors and social determinants of health. They reflect the health status of a community.
- Mortality: This category includes measures of death rates.
- Infant mortality rates: This metric measures the number of infant deaths per 1,000 live births.
- Premature death rates: This metric measures the number of deaths before the age of 75 per 100,000 people.
- Morbidity: This category includes measures of illness and disability.
- Rates of chronic diseases: This metric measures the prevalence of chronic diseases, such as heart disease, cancer, and diabetes.
- Rates of preventable hospitalizations: This metric measures the number of hospitalizations that could have been prevented through better access to healthcare.
- Quality of Life: This category includes measures of overall well-being.
- Self-reported health status: This metric measures how people rate their own health.
- Mental health: This metric measures the prevalence of mental health problems, such as depression and anxiety.
- Life satisfaction: This metric measures how satisfied people are with their lives.
Social Determinants of Health, County health rankings
Social determinants of health are the conditions in which people are born, grow, live, work, and age. They are the factors that influence health outcomes.
- Education: This category includes measures of educational attainment.
- High school graduation rates: This metric measures the percentage of adults who have completed high school.
- College graduation rates: This metric measures the percentage of adults who have completed college.
- Income: This category includes measures of income and wealth.
- Median household income: This metric measures the average income of households in a community.
- Poverty rates: This metric measures the percentage of people living below the poverty line.
- Income inequality: This metric measures the gap between the richest and poorest members of a community.
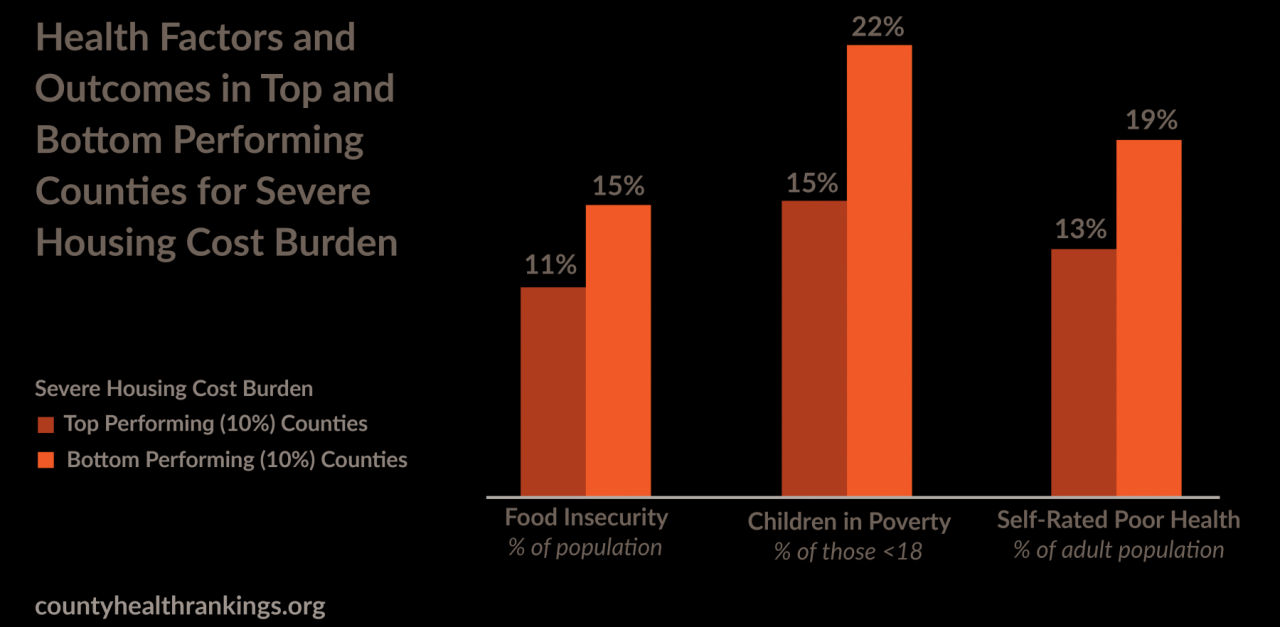
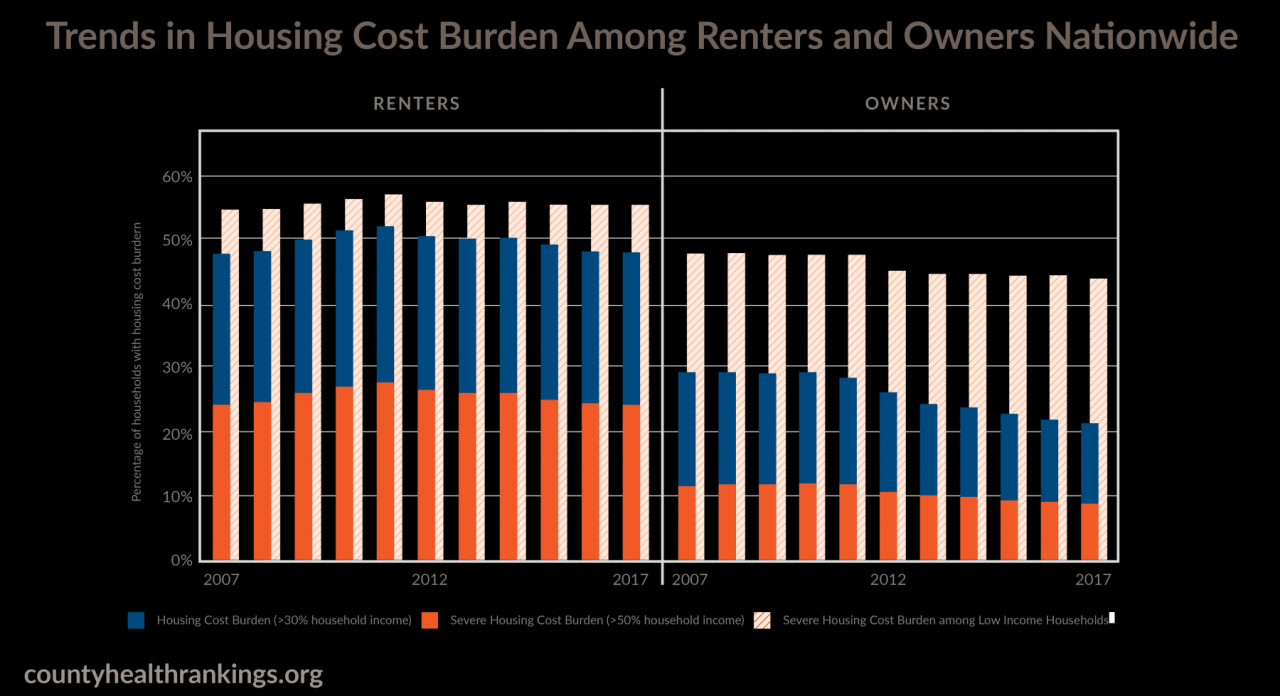
- Housing: This category includes measures of housing quality and affordability.
- Housing costs: This metric measures the percentage of income spent on housing.
- Homeownership rates: This metric measures the percentage of households that own their home.
- Overcrowding: This metric measures the number of people living in a household per bedroom.
- Transportation: This category includes measures of access to transportation.
- Car ownership: This metric measures the percentage of households that own a car.
- Access to public transportation: This metric measures the availability of public transportation in a community.
- Walkability: This metric measures the ease of walking in a community.
Policy Factors
Policy factors are laws, regulations, and programs that influence health.
- Health Policies: This category includes policies related to healthcare access and quality.
- Medicaid expansion: This policy expands Medicaid coverage to more low-income adults.
- State tobacco taxes: This policy increases the price of cigarettes.
- Minimum legal drinking age: This policy sets the minimum age for purchasing and consuming alcohol.
- Social Policies: This category includes policies related to education, income, and housing.
- Early childhood education: This policy provides early education programs for children.
- Minimum wage: This policy sets the minimum wage that employers must pay their workers.
- Affordable housing programs: This policy provides affordable housing options for low-income families.
- Environmental Policies: This category includes policies related to air and water quality.
- Air quality standards: This policy sets limits on the amount of air pollution allowed.
- Clean water regulations: This policy sets standards for the quality of drinking water.
- Recycling programs: This policy encourages recycling to reduce waste.
Factors Influencing County Health
County health rankings are influenced by a complex interplay of factors that affect the well-being of residents. These factors go beyond just healthcare access and encompass a wide range of social, economic, and environmental determinants that shape health outcomes.
Social Determinants of Health, County health rankings
Social determinants of health are the conditions in which people are born, grow, live, work, and age. These factors can significantly influence health outcomes and contribute to health disparities across counties.
- Education: Education levels are strongly correlated with health outcomes. Higher levels of education are associated with better health behaviors, greater access to information, and higher incomes, leading to improved health outcomes.
- Social and Community Context: The social and community context, including social cohesion, safety, and access to social support networks, plays a crucial role in shaping health. Strong social connections and supportive communities contribute to better mental and physical health.
- Economic Stability: Economic stability, including employment, income, and housing security, is a significant determinant of health. Poverty and unemployment are associated with increased stress, limited access to healthcare, and poorer health outcomes.
Economic Factors
Economic factors play a crucial role in shaping county health rankings. Poverty and unemployment, for instance, can have a profound impact on health outcomes.
- Poverty: Poverty is a major driver of poor health. Individuals living in poverty often face limited access to nutritious food, safe housing, and healthcare, leading to higher rates of chronic diseases and premature mortality.
- Unemployment: Unemployment can lead to financial stress, social isolation, and reduced access to healthcare, all of which contribute to poorer health outcomes.
Environmental Factors
Environmental factors, including air and water quality, can significantly impact county health.
- Air Quality: Exposure to air pollution, particularly from vehicle emissions and industrial activity, can contribute to respiratory problems, heart disease, and other health issues.
- Water Quality: Access to clean and safe drinking water is essential for good health. Contaminated water sources can lead to waterborne diseases and other health problems.
Healthcare Access and Quality
Access to quality healthcare services is crucial for maintaining good health and preventing disease.
- Healthcare Access: Limited access to healthcare services, including primary care, specialty care, and preventive services, can lead to delayed diagnoses, untreated health conditions, and poorer health outcomes.
- Healthcare Quality: The quality of healthcare services, including the skills and training of healthcare providers, the availability of advanced medical technology, and the overall efficiency of the healthcare system, can influence health outcomes.
Trends and Patterns in County Health

The County Health Rankings provide a valuable snapshot of health status across the United States, but examining trends over time reveals crucial insights into the dynamic nature of health outcomes and the factors that influence them. By analyzing historical data, we can identify patterns and disparities in health, providing a foundation for informed policy decisions and targeted interventions.
Historical Trends in County Health Rankings
Examining trends in county health rankings over time provides a valuable perspective on the evolution of health outcomes across the nation.
County health rankings can provide valuable insights into the overall well-being of a community, highlighting areas where improvement is needed. Access to affordable fitness options, like those offered by Planet Fitness, can play a crucial role in boosting community health.
You can find great deals on Planet Fitness memberships with a planet fitness coupons code , making it easier for residents to prioritize their physical well-being. Ultimately, improving access to fitness resources can contribute to a healthier population and higher county health rankings.
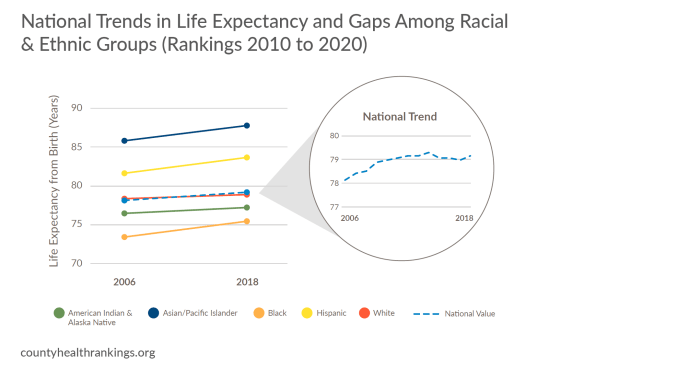
- Overall Health Status:The overall health status of counties in the United States has shown gradual improvement over the past decade. This improvement is reflected in increasing life expectancy and decreasing rates of premature death.
- Health Factors:There are notable trends in specific health factors that contribute to overall health. For example, rates of smoking have declined significantly, while obesity rates have remained relatively stable.
- Health Outcomes:Trends in health outcomes, such as heart disease, stroke, and cancer, vary across counties and over time.
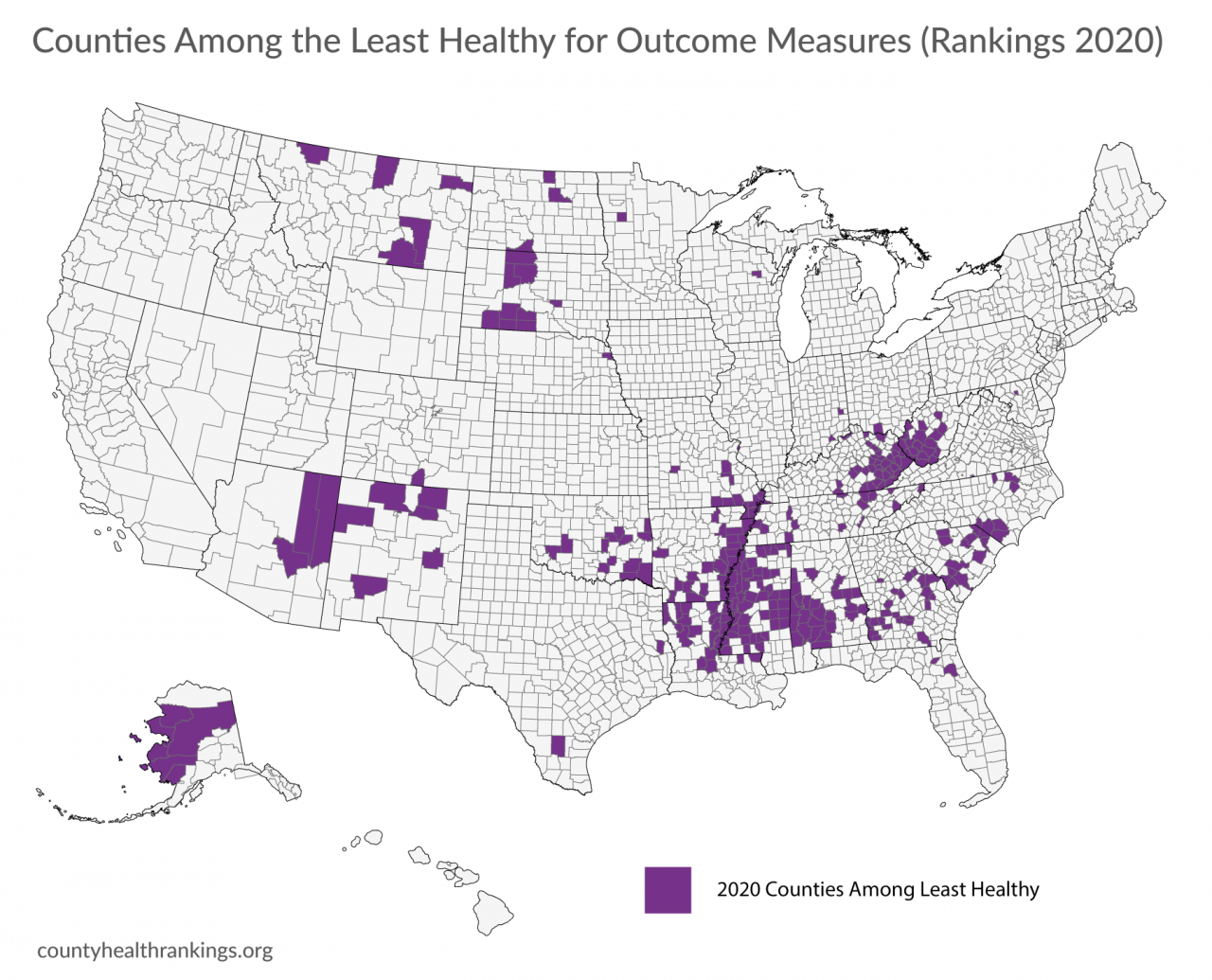
Geographic Patterns and Disparities in Health Outcomes
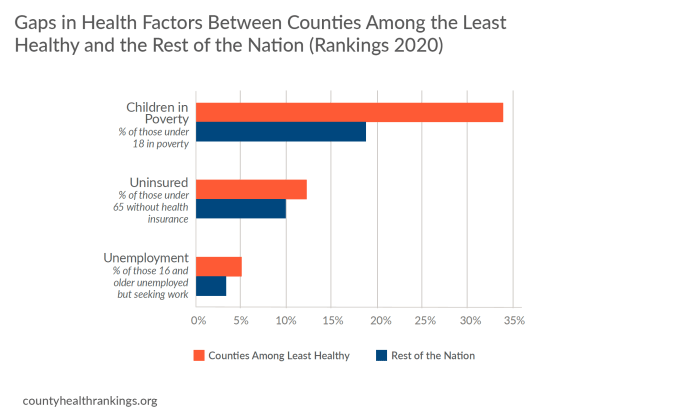
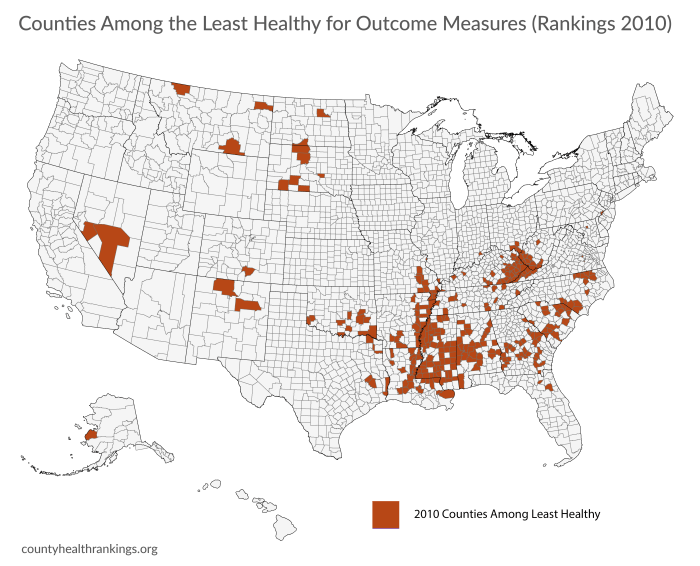
County health rankings reveal distinct geographic patterns and disparities in health outcomes across the United States.
- Rural vs. Urban Health:Rural counties often experience poorer health outcomes compared to urban counties. This disparity is attributed to factors such as limited access to healthcare, lower socioeconomic status, and higher rates of chronic diseases.
- Racial and Ethnic Disparities:Persistent racial and ethnic disparities in health outcomes are evident in county health rankings. These disparities are rooted in systemic inequities in access to healthcare, education, and economic opportunities.
- Regional Variations:Significant regional variations in health outcomes exist across the United States. These variations are influenced by factors such as climate, environmental conditions, and cultural practices.
Potential Causes of Observed Trends and Disparities
The trends and disparities observed in county health rankings are influenced by a complex interplay of factors.
- Socioeconomic Factors:Factors such as poverty, unemployment, and lack of education are strongly associated with poor health outcomes.
- Environmental Factors:Exposure to environmental hazards, such as air pollution and contaminated water, can negatively impact health.
- Healthcare Access and Quality:Limited access to quality healthcare, including preventive services, contributes to health disparities.
- Social Determinants of Health:Factors such as housing, transportation, and food security play a crucial role in shaping health outcomes.
Strategies for Improving County Health: County Health Rankings

Improving county health requires a multi-faceted approach that addresses the complex factors influencing health outcomes. Strategies can be categorized into different areas, each targeting specific aspects of the social, economic, and environmental determinants of health.
Strategies for Improving County Health
A comprehensive approach to improving county health involves various strategies that can be implemented at different levels, from individual behaviors to community-level interventions. The table below provides a framework for understanding these strategies and their potential impact on county health outcomes.
| Strategy | Description | Examples | Challenges | Opportunities |
|---|---|---|---|---|
| Health Education and Promotion | Promoting healthy behaviors and increasing awareness of health risks. | Public awareness campaigns on smoking cessation, nutrition education programs, and physical activity initiatives. | Limited access to resources, low health literacy, and cultural barriers. | Partnerships with community organizations, use of technology for health education, and tailored messaging. |
| Access to Quality Healthcare | Ensuring affordable and accessible healthcare services for all residents. | Expanding access to primary care, mental health services, and preventive screenings. | High healthcare costs, provider shortages, and transportation barriers. | Telehealth services, community health centers, and mobile clinics. |
| Economic Opportunities and Social Determinants of Health | Addressing factors that contribute to socioeconomic disparities in health, such as poverty, unemployment, and lack of education. | Job training programs, affordable housing initiatives, and community development projects. | Limited funding, lack of political will, and complex social systems. | Collaboration with local businesses, community-based organizations, and government agencies. |
| Environmental Health and Safety | Protecting residents from environmental hazards that impact health, such as air and water pollution. | Enhancing air quality regulations, promoting safe drinking water, and reducing exposure to lead. | Limited resources for environmental monitoring and enforcement, lack of public awareness, and industry resistance. | Public-private partnerships, community engagement, and environmental justice initiatives. |
| Community Health and Wellness | Building healthy communities through social connections, community infrastructure, and supportive environments. | Creating parks and green spaces, promoting active transportation, and fostering community cohesion. | Limited funding, lack of community involvement, and competing priorities. | Partnerships with community organizations, neighborhood-based initiatives, and social media campaigns. |
Successful Interventions
Several counties have implemented successful interventions that have improved health outcomes. These interventions demonstrate the effectiveness of various strategies in addressing specific health challenges.
- Cook County, Illinois:Implemented a comprehensive program to address the opioid epidemic, including expanding access to treatment, providing naloxone to first responders, and promoting prevention efforts. This program has led to a significant decrease in opioid overdose deaths.
- San Diego County, California:Established a countywide health equity plan that focuses on addressing disparities in health outcomes based on race, ethnicity, and socioeconomic status. The plan has resulted in improved access to healthcare services and community resources for underserved populations.
- King County, Washington:Implemented a countywide tobacco control program that includes smoke-free policies, tobacco cessation programs, and public awareness campaigns. This program has led to a significant decline in smoking rates and improved air quality.
Challenges and Opportunities
Implementing strategies for improving county health faces various challenges and opportunities. Understanding these factors is crucial for effective program design and implementation.
- Funding:Securing adequate funding for health programs is a significant challenge, especially in counties with limited resources. This requires creative approaches to funding, such as leveraging federal and state grants, partnering with private organizations, and exploring alternative funding sources.
- Political Will:Political support is essential for implementing and sustaining health programs. Building consensus among elected officials and community leaders requires effective advocacy, public education, and engagement with stakeholders.
- Data and Evaluation:Measuring the impact of health programs is crucial for demonstrating their effectiveness and identifying areas for improvement. This requires robust data collection systems, rigorous evaluation methods, and transparent reporting of results.
- Community Engagement:Engaging community members in the design, implementation, and evaluation of health programs is essential for ensuring their relevance and sustainability. This requires building trust, fostering collaboration, and empowering communities to take ownership of their health.
The Role of Public Health Agencies
Public health agencies play a crucial role in promoting and protecting the health of communities. They are responsible for implementing a wide range of programs and initiatives aimed at improving the health of residents, including addressing health disparities, promoting healthy behaviors, and preventing disease outbreaks.
Impact of Public Health Programs and Initiatives
Public health programs and initiatives have a significant impact on county health rankings. These programs address various health issues, such as chronic diseases, infectious diseases, and environmental hazards. By implementing evidence-based interventions, public health agencies can improve health outcomes, reduce health disparities, and enhance the overall well-being of communities.
- Immunization programs:Public health agencies administer vaccination programs to protect individuals from preventable diseases. Immunization programs have significantly reduced the incidence of vaccine-preventable diseases, such as measles, mumps, and rubella, contributing to improved health outcomes and increased life expectancy. For example, the Centers for Disease Control and Prevention (CDC) estimates that vaccination has prevented over 21 million hospitalizations and 732,000 deaths among children born in the last 20 years.
- Health education campaigns:Public health agencies conduct health education campaigns to raise awareness about health risks and promote healthy behaviors. These campaigns can target specific populations, such as youth, pregnant women, or individuals with chronic conditions. For instance, public health agencies have launched successful campaigns to promote tobacco cessation, increase physical activity, and improve nutrition.
- Disease surveillance and outbreak response:Public health agencies monitor disease trends and respond to outbreaks of infectious diseases. By tracking disease patterns and identifying potential outbreaks, public health agencies can implement timely interventions to prevent the spread of diseases and protect public health. For example, during the COVID-19 pandemic, public health agencies played a critical role in implementing testing, contact tracing, and vaccination programs to mitigate the impact of the virus.
Collaboration with Other Stakeholders
Effective public health programs require collaboration between public health agencies and other stakeholders, such as healthcare providers, schools, businesses, and community organizations. This collaboration is essential for implementing comprehensive strategies that address the multifaceted determinants of health.
Collaboration is key to addressing complex health issues and achieving lasting improvements in county health rankings.
- Healthcare providers:Public health agencies work closely with healthcare providers to promote disease prevention, early detection, and management of chronic conditions. This collaboration can involve sharing data, coordinating services, and developing joint initiatives to improve patient care.
- Schools:Public health agencies collaborate with schools to promote healthy behaviors among children and adolescents. This collaboration can involve providing health education programs, implementing nutrition guidelines, and promoting physical activity.
- Businesses:Public health agencies work with businesses to create healthier workplaces and promote employee well-being. This collaboration can involve implementing workplace wellness programs, promoting healthy eating options, and encouraging physical activity.
- Community organizations:Public health agencies partner with community organizations to reach underserved populations and address health disparities. This collaboration can involve providing health education, promoting access to healthcare, and supporting community-based initiatives.
Community Engagement and Health Equity
Community engagement is crucial for improving county health. When communities are actively involved in shaping health initiatives, they are more likely to be successful and sustainable. By understanding the unique needs and challenges of a community, public health agencies can tailor programs and services to be more effective and relevant.
Strategies for Addressing Health Disparities and Promoting Health Equity
Health disparities are preventable differences in health outcomes that are experienced by certain population groups. These disparities are often rooted in social, economic, and environmental factors that contribute to unequal access to healthcare, healthy food, safe housing, and other essential resources.
Addressing these disparities and promoting health equity requires a multifaceted approach that considers the root causes of these inequities.
- Data Collection and Analysis:Gathering and analyzing data on health disparities is essential for identifying the specific populations that are experiencing inequities and understanding the underlying factors that contribute to these disparities. This data can then be used to develop targeted interventions and programs.
- Community-Based Participatory Research (CBPR):CBPR involves working collaboratively with community members to design, conduct, and interpret research. This approach ensures that research is relevant to the community’s needs and priorities, and it empowers community members to become active participants in the research process.
- Culturally and Linguistically Appropriate Services (CLAS):CLAS refers to providing healthcare services that are respectful of cultural differences and linguistic needs. This includes offering services in multiple languages, using culturally appropriate materials and communication styles, and ensuring that staff are trained to provide culturally competent care.
- Addressing Social Determinants of Health:Social determinants of health are the conditions in which people are born, grow, live, work, and age. These factors can have a profound impact on health outcomes. Strategies to address these determinants include promoting economic opportunity, improving access to education, providing affordable housing, and creating safe and healthy environments.
- Building Partnerships:Working collaboratively with community organizations, faith-based institutions, schools, and other stakeholders is essential for reaching underserved populations and addressing the social determinants of health.
Examples of Community-Based Initiatives
Many community-based initiatives have successfully improved health outcomes by engaging community members in the design, implementation, and evaluation of programs.
County health rankings offer a valuable snapshot of the well-being of communities, highlighting areas that need attention and improvement. It’s important to remember that true beauty lies not just in physical appearance but also in overall health and vitality, which is something that can be nurtured and fostered.
By understanding the factors that contribute to a healthy community, we can work towards creating environments that support truly beauty for everyone. Ultimately, these rankings serve as a call to action to prioritize health and well-being in our communities.
- Community Health Workers (CHWs):CHWs are trusted members of the community who provide health education, outreach, and support services. They are often able to reach underserved populations and build relationships that foster trust and improve health outcomes.
- Food Access Initiatives:Programs that address food insecurity and improve access to healthy foods, such as community gardens, farmers’ markets, and food banks, can have a significant impact on health outcomes.
- Health Education and Promotion Campaigns:Engaging community members in the development and implementation of health education and promotion campaigns can ensure that messages are culturally relevant and resonate with the target audience.
Future Directions for County Health Rankings
The County Health Rankings provide a valuable framework for understanding and addressing health disparities across the nation. As we move forward, it is essential to continue to refine and expand these rankings to ensure they remain relevant and impactful. This section explores potential future directions for county health rankings, emphasizing the need for continuous data collection and analysis, identifying emerging health challenges and opportunities for intervention.
Continuous Data Collection and Analysis
The County Health Rankings rely on a robust dataset of health indicators, socioeconomic factors, and environmental conditions. To maintain the accuracy and relevance of these rankings, it is crucial to engage in ongoing data collection and analysis. This includes:
- Expanding the Scope of Data:The rankings can be enhanced by incorporating additional health indicators, such as mental health, access to healthy food, and environmental factors like air quality. This broader perspective would provide a more comprehensive understanding of county health.
- Improving Data Quality and Availability:Ensuring the accuracy, completeness, and timeliness of data is essential. This may involve working with data providers to improve data collection methods and enhance data sharing initiatives.
- Developing Innovative Data Analysis Techniques:Utilizing advanced statistical methods and data visualization tools can help identify trends, patterns, and potential causal relationships within the data. This can inform the development of targeted interventions and policies.
Emerging Health Challenges and Opportunities for Intervention
The health landscape is constantly evolving, presenting new challenges and opportunities for intervention. County health rankings can play a vital role in identifying and addressing these emerging issues. Examples include:
- The Opioid Crisis:The rankings can be used to monitor the prevalence of opioid use disorder and overdose deaths at the county level. This data can inform the development of targeted prevention and treatment programs, as well as policies to reduce access to opioids.
- Climate Change and Health:Climate change is expected to have significant impacts on health, including increased heat-related illnesses, respiratory problems, and the spread of infectious diseases. The rankings can be used to assess county-level vulnerability to these health risks and identify strategies for adaptation and mitigation.
- Social Determinants of Health:The rankings can be used to explore the impact of social determinants of health, such as poverty, education, and access to transportation, on health outcomes. This data can inform policies and programs that address these underlying factors.
Concluding Remarks
County Health Rankings play a crucial role in driving positive change by providing valuable data and insights. By fostering collaboration among stakeholders, promoting community engagement, and prioritizing health equity, we can leverage the information gleaned from these rankings to create healthier communities for all.
The future of county health rankings holds immense promise, as ongoing data collection and analysis pave the way for more effective interventions and a deeper understanding of the multifaceted factors that shape health outcomes.
Detailed FAQs
What are the benefits of using County Health Rankings?
County Health Rankings provide a valuable tool for understanding health trends, identifying areas for improvement, and promoting community engagement in health initiatives.
How can I use County Health Rankings to improve my community’s health?
You can use the rankings to advocate for policies and programs that address key health indicators, support community-based initiatives, and promote health equity.
Are there any limitations to County Health Rankings?
While the rankings offer valuable insights, they should be considered within the context of broader social and economic factors. It’s important to recognize that rankings are a snapshot in time and may not capture all aspects of health.