Inequalities health – Inequalities in health are a pressing global issue, highlighting the stark disparities in health outcomes across populations. These disparities are not merely random occurrences but are rooted in complex social, economic, and environmental factors that create unequal access to healthcare, education, and other resources.
From the cradle to the grave, health inequalities manifest in various ways, affecting individuals and communities alike. This exploration delves into the multifaceted nature of health inequalities, examining their causes, consequences, and potential solutions.
Defining Health Inequalities
Health inequalities refer to the avoidable and unfair differences in health status between different groups of people within a society. These inequalities are not just about disparities in health outcomes, but also about the underlying social, economic, and environmental factors that contribute to these differences.
Health Inequalities vs. Health Disparities
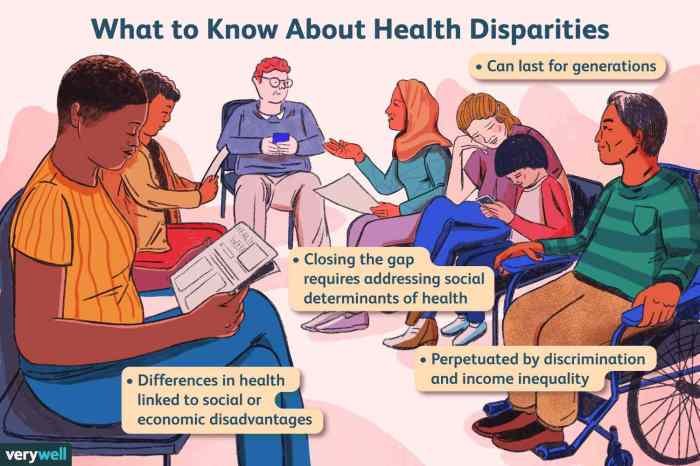
The terms “health inequalities” and “health disparities” are often used interchangeably, but they have distinct meanings. While both refer to differences in health outcomes, health disparities focus on the differences in health status between groups based on specific characteristics like race, ethnicity, gender, or socioeconomic status.
Health inequalities, on the other hand, emphasize the unfairnessand avoidabilityof these differences, highlighting the social and economic factors that create and perpetuate them.
Inequalities in health can be exacerbated by limited access to affordable fitness options. In Sioux Falls, South Dakota, Crunch Fitness Sioux Falls offers a variety of membership options, which can be a positive step towards improving overall health and well-being, especially for those who may face financial barriers to fitness.
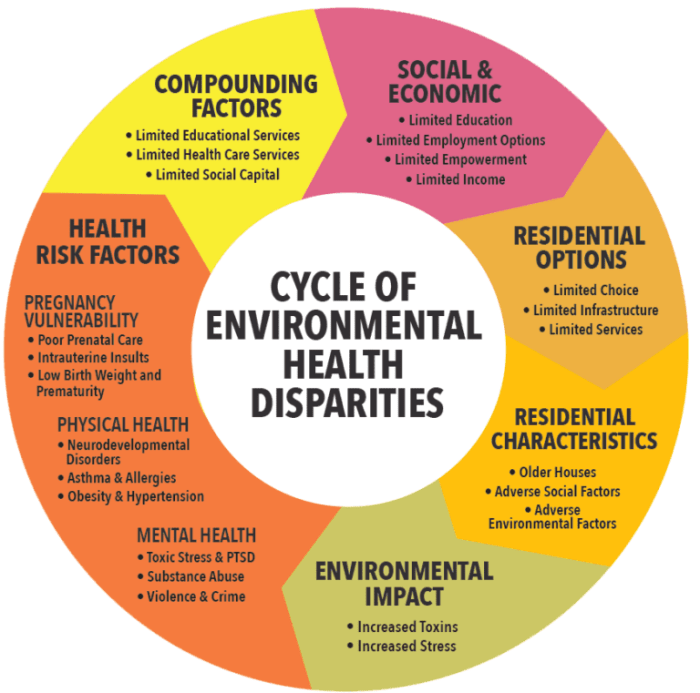
Social Determinants of Health, Inequalities health
The social determinants of health (SDOH) are the non-medical factors that influence an individual’s health status. These factors include:
- Economic stability:Income, employment, and access to affordable housing can significantly impact health outcomes. For example, individuals living in poverty may experience higher rates of chronic diseases due to limited access to healthy food, healthcare, and safe living environments.
- Education:Educational attainment is strongly linked to health outcomes. Individuals with higher levels of education tend to have better health habits, access to better jobs, and higher incomes, all of which contribute to improved health.
- Social and community context:Social support networks, community safety, and access to social services can influence health outcomes. For example, individuals living in communities with high crime rates or limited access to healthcare may experience poorer health.
- Healthcare access and quality:Access to affordable and quality healthcare services is crucial for maintaining good health. Inequalities in access to healthcare can lead to disparities in health outcomes.
- Neighborhood and built environment:The physical environment where people live, work, and play can influence their health. Factors such as air and water quality, access to green spaces, and transportation options can impact health outcomes.
Types of Health Inequalities
Health inequalities manifest in various ways, often intersecting across different social groups. Some common examples include:
- Racial and ethnic inequalities:People of color often experience worse health outcomes than their white counterparts due to systemic racism, discrimination, and lack of access to resources.
- Socioeconomic inequalities:Individuals with lower socioeconomic status are more likely to experience poor health due to factors like limited access to healthcare, education, and healthy food.
- Gender inequalities:Women often face unique health challenges, including higher rates of certain diseases and disparities in access to healthcare.
- Geographic inequalities:People living in rural areas or underserved communities may have limited access to healthcare, healthy food, and other essential services, leading to poorer health outcomes.
Health Inequalities Across the Lifespan

Health inequalities are not confined to a specific age group; they manifest differently across the lifespan, impacting individuals at various stages of life. Understanding these disparities is crucial for developing targeted interventions and promoting health equity.
Health Inequalities in Childhood
Children are particularly vulnerable to health inequalities, as they are still developing physically, mentally, and emotionally. These inequalities can have lasting consequences on their health and well-being.
- Socioeconomic Status:Children from low-income families are more likely to experience poor health outcomes due to factors such as inadequate nutrition, limited access to healthcare, and exposure to environmental hazards. For instance, a study published in the journal “Pediatrics” found that children living in poverty are more likely to have chronic health conditions, such as asthma and obesity, compared to their wealthier counterparts.
- Race and Ethnicity:Racial and ethnic disparities in health are also prevalent in childhood. For example, Black and Hispanic children are more likely to experience higher rates of infant mortality and childhood obesity compared to white children. These disparities are often attributed to systemic racism and discrimination, which can limit access to quality healthcare and resources.
- Geographic Location:Children living in rural areas or disadvantaged neighborhoods may face limited access to healthcare services, educational opportunities, and healthy food options. This can lead to poorer health outcomes and limit their future opportunities. A study published in the “Journal of Rural Health” found that children living in rural areas have higher rates of chronic diseases, such as diabetes and heart disease, compared to children living in urban areas.
Health Inequalities in Adolescence
Adolescence is a critical period for physical, mental, and social development, and health inequalities during this time can have significant long-term consequences.
- Mental Health:Adolescents from disadvantaged backgrounds are more likely to experience mental health problems, such as depression, anxiety, and substance abuse. This can be attributed to factors such as poverty, discrimination, and lack of access to mental health services. For example, a study published in the “Journal of Adolescent Health” found that adolescents living in poverty are more likely to experience depression and anxiety compared to their wealthier peers.
- Sexual and Reproductive Health:Access to sexual and reproductive healthcare services can vary significantly based on socioeconomic status, race, and ethnicity. Adolescents from disadvantaged backgrounds may face barriers to obtaining contraception, STI testing, and other essential services, which can lead to unintended pregnancies and sexually transmitted infections.
- Education and Employment:Health inequalities can also impact educational and employment opportunities for adolescents. For instance, adolescents from low-income families may be more likely to drop out of school or struggle to find employment due to health issues or lack of access to resources.
This can have a cascading effect on their future health and well-being.
Health Inequalities in Adulthood
Health inequalities continue to persist throughout adulthood, with significant implications for overall health and well-being.
- Chronic Diseases:Adults from disadvantaged backgrounds are more likely to develop chronic diseases, such as heart disease, stroke, diabetes, and cancer. This is often attributed to factors such as poor diet, lack of physical activity, smoking, and limited access to healthcare.
For example, a study published in the “American Journal of Public Health” found that adults living in poverty are more likely to have diabetes and heart disease compared to their wealthier counterparts.
- Workplace Hazards:Individuals working in hazardous or stressful jobs may be exposed to occupational hazards that can lead to health problems. These hazards can include exposure to chemicals, physical strain, and psychological stress. For instance, a study published in the “Journal of Occupational and Environmental Medicine” found that workers in certain industries, such as construction and manufacturing, are more likely to develop musculoskeletal disorders and respiratory illnesses.
- Social Determinants of Health:Social determinants of health, such as education, income, housing, and access to transportation, play a significant role in health outcomes during adulthood. Individuals with lower socioeconomic status are more likely to experience poor health due to limited access to resources and opportunities.
Health Inequalities in Older Adulthood
Older adults are particularly vulnerable to health inequalities, as they are more likely to experience chronic diseases and disabilities.
- Chronic Diseases and Disabilities:Older adults from disadvantaged backgrounds are more likely to experience chronic diseases, such as arthritis, heart disease, and dementia. They are also more likely to have disabilities that limit their mobility and independence. These health issues can lead to social isolation, decreased quality of life, and increased healthcare costs.
- Access to Healthcare:Older adults from low-income families may face barriers to accessing healthcare services due to limited financial resources, lack of transportation, or inadequate insurance coverage. This can result in delayed diagnosis and treatment, leading to poorer health outcomes.
- Long-Term Care:Older adults with chronic illnesses or disabilities may require long-term care services, such as assisted living or nursing home care. Access to these services can vary significantly based on socioeconomic status, race, and ethnicity. Individuals from disadvantaged backgrounds may have limited access to quality long-term care, leading to poorer health outcomes and increased costs.
Impact of Health Inequalities on Individuals and Communities

Health inequalities have a profound and multifaceted impact, extending beyond individual health outcomes to encompass societal well-being and economic prosperity. Understanding the ramifications of these disparities is crucial for developing effective interventions and fostering a more equitable society.
Impact on Individual Health Outcomes
The consequences of health inequalities on individuals are far-reaching, affecting their life expectancy, morbidity, and overall quality of life.
- Reduced Life Expectancy:Individuals from disadvantaged socioeconomic backgrounds often experience shorter life spans compared to their more affluent counterparts. This disparity can be attributed to factors such as limited access to quality healthcare, exposure to environmental hazards, and unhealthy lifestyle choices driven by socioeconomic constraints.
- Increased Morbidity:Health inequalities lead to higher rates of chronic diseases, such as heart disease, diabetes, and cancer, among marginalized populations. This increased morbidity is often linked to factors like poor nutrition, lack of physical activity, and exposure to environmental stressors.
- Impaired Quality of Life:Health inequalities can significantly impact individuals’ quality of life, leading to limitations in their ability to work, participate in social activities, and enjoy their lives to the fullest. Chronic illnesses, disability, and premature mortality can all contribute to a diminished quality of life.
Social and Economic Consequences for Communities
The impact of health inequalities extends beyond individual well-being, affecting entire communities and their social and economic fabric.
- Increased Healthcare Costs:Health inequalities drive up healthcare costs for communities. Higher rates of chronic diseases and preventable conditions among disadvantaged populations place a significant burden on healthcare systems, requiring increased spending on treatments, hospitalizations, and long-term care.
- Reduced Workforce Productivity:Health inequalities can lead to lower workforce productivity. Chronic illnesses, disability, and premature mortality among disadvantaged populations can reduce the overall economic output of communities. This loss of productivity can have a ripple effect on businesses, industries, and the overall economy.
- Erosion of Social Cohesion:Health inequalities can contribute to social divisions and erode social cohesion within communities. When certain groups experience significantly poorer health outcomes, it can lead to feelings of resentment, distrust, and social isolation. This can undermine community spirit and make it more difficult to address shared challenges.
Health Inequalities and Social Mobility
Health inequalities can have a significant impact on social mobility, perpetuating cycles of poverty and disadvantage.
- Limited Educational Opportunities:Poor health can hinder educational attainment, limiting opportunities for social mobility. Children from disadvantaged backgrounds may face challenges in school due to health issues, leading to lower academic performance and reduced chances of pursuing higher education.
- Reduced Employment Prospects:Health inequalities can lead to lower employment prospects and reduced earnings. Chronic illnesses, disability, and premature mortality can all limit individuals’ ability to participate in the workforce and achieve economic stability. This can trap individuals and their families in cycles of poverty and limit their ability to improve their social standing.
- Intergenerational Transmission of Disadvantage:Health inequalities can be passed down through generations, perpetuating cycles of poverty and disadvantage. Children born into disadvantaged families may inherit poor health outcomes, limited access to resources, and reduced opportunities, making it difficult for them to break free from the cycle of deprivation.
Health inequalities are a persistent problem, with certain groups facing disproportionate challenges accessing quality care. This disparity is particularly evident in the realm of long-term care, where individuals requiring specialized support often struggle to find adequate resources. Advanced care home health, such as those offered by healthbeautynfitness.com , can play a crucial role in bridging this gap by providing personalized and comprehensive care tailored to individual needs, ultimately contributing to a more equitable healthcare system.
Addressing Health Inequalities
Addressing health inequalities is a complex and multifaceted challenge that requires a comprehensive approach involving various stakeholders. It’s essential to acknowledge that health disparities are not inevitable but rather the result of social, economic, and environmental factors that can be addressed through targeted interventions and policy changes.
Strategies and Interventions to Address Health Inequalities
A wide range of strategies and interventions can be employed to address health inequalities. These strategies target different aspects of the problem, from individual behavior change to systemic policy reforms. The effectiveness of these strategies can vary depending on the specific context and target population.
| Strategy | Target Population | Potential Benefits | Challenges |
|---|---|---|---|
| Early childhood interventions | Children from disadvantaged backgrounds | Improved cognitive development, reduced risk of chronic diseases, increased educational attainment | High costs, potential for unintended consequences, difficulty reaching all children in need |
| Health education and promotion campaigns | Individuals at risk of developing health problems | Increased awareness of health risks, improved health behaviors, reduced incidence of preventable diseases | Limited reach, difficulty changing ingrained behaviors, potential for stigma and blame |
| Community-based health programs | Individuals and communities with limited access to healthcare | Improved access to healthcare services, increased health literacy, enhanced community support | Funding challenges, difficulty coordinating with existing healthcare systems, potential for program duplication |
| Policy reforms | Population as a whole | Reduced socioeconomic disparities, improved living conditions, increased access to healthcare | Political resistance, difficulty implementing complex policies, potential for unintended consequences |
| Social safety net programs | Individuals and families living in poverty | Reduced poverty, improved food security, increased access to education and healthcare | High costs, potential for program abuse, difficulty reaching all those in need |
Public Health Campaign to Reduce Health Inequalities
A public health campaign aimed at reducing health inequalities could target a diverse audience, including policymakers, healthcare providers, community leaders, and the general public. The campaign’s key messages should focus on raising awareness of health inequalities, promoting social justice, and advocating for policies that promote health equity.
The campaign could utilize various communication channels, such as:
- Social media platforms like Facebook, Twitter, and Instagram to reach a wide audience and engage in interactive discussions.
- Television and radio advertisements to reach a broader audience and increase public awareness.
- Community events and workshops to engage with local communities and promote dialogue on health inequalities.
- Educational materials and resources to provide information and empower individuals to advocate for change.
The campaign should also emphasize the importance of individual responsibility while acknowledging the systemic factors that contribute to health disparities. It should promote messages of hope and empowerment, highlighting the positive impact that collective action can have on reducing health inequalities.
Role of Policy, Healthcare Systems, Community Engagement, and Individual Behavior Change
Addressing health inequalities requires a multi-pronged approach that involves policy changes, healthcare system reforms, community engagement, and individual behavior change.
Policyplays a crucial role in creating a level playing field and addressing the root causes of health disparities. This includes policies that promote economic equality, ensure access to quality education and housing, and address environmental hazards. For example, policies that guarantee paid sick leave, affordable housing, and access to quality childcare can have a significant impact on health outcomes.
Healthcare systemsmust be designed to meet the needs of all individuals, regardless of their socioeconomic status. This includes expanding access to primary care, providing culturally competent services, and addressing health disparities within healthcare delivery. For example, ensuring that healthcare providers are adequately trained to address the needs of diverse populations and that healthcare services are culturally sensitive can help improve health outcomes for marginalized groups.
Community engagementis essential for identifying local health needs, developing culturally appropriate interventions, and mobilizing community resources. This includes working with community leaders, faith-based organizations, and local residents to address health disparities at the grassroots level. For example, community-based health programs that address specific health concerns, such as diabetes or obesity, can be effective in improving health outcomes for marginalized communities.
Individual behavior changeis also important, but it must be addressed within the context of social and environmental factors that influence health choices. This includes promoting healthy behaviors, such as regular exercise, healthy eating, and smoking cessation, while addressing the barriers that prevent individuals from making healthy choices.
Health inequalities are a significant issue, with access to resources like fitness facilities playing a crucial role. For example, a membership at LA Fitness could provide access to a pool, offering a low-impact exercise option that benefits individuals with mobility limitations or specific health concerns.
Addressing these disparities requires creating equitable access to such resources, ensuring everyone has a fair chance to improve their health and well-being.
For example, providing access to healthy and affordable food options, creating safe spaces for physical activity, and supporting individuals to quit smoking can all contribute to individual behavior change.
Measuring and Monitoring Health Inequalities
To effectively address health inequalities, it is crucial to measure and monitor them accurately. This involves using various methods to collect, analyze, and interpret data on health disparities.
Methods for Measuring and Monitoring Health Inequalities
There are several key methods used to measure and monitor health inequalities:
- Health Indicators:These are quantifiable measures that reflect the health status of a population. Examples include life expectancy, infant mortality rate, and prevalence of chronic diseases. By comparing these indicators across different socioeconomic groups, researchers can identify disparities in health outcomes.
- Data Collection:Comprehensive data collection is essential for understanding health inequalities. This involves gathering information from various sources, including:
- Surveys:Large-scale surveys, such as the National Health Interview Survey (NHIS) in the United States, collect detailed data on health status, access to care, and socioeconomic factors.
- Administrative Data:Data from health insurance claims, hospital discharge records, and death certificates can be used to track health outcomes and identify disparities.
- Geographic Information Systems (GIS):GIS technology can be used to map health indicators and socioeconomic factors, allowing researchers to identify areas with high concentrations of health inequalities.
- Statistical Analysis:Statistical methods are used to analyze collected data and identify significant differences in health outcomes between groups. Techniques such as regression analysis can help determine the association between socioeconomic factors and health disparities.
Key Health Indicators for Assessing Health Inequalities
| Indicator | Definition | Measurement | Data Sources |
|---|---|---|---|
| Life Expectancy | Average number of years a person is expected to live at birth. | Years | National vital statistics, population surveys |
| Infant Mortality Rate | Number of deaths of infants under one year of age per 1,000 live births. | Deaths per 1,000 live births | National vital statistics |
| Prevalence of Chronic Diseases | Proportion of the population with a specific chronic disease, such as diabetes or heart disease. | Percentage of the population | Health surveys, administrative data |
| Health Disparities in Access to Care | Differences in access to healthcare services based on socioeconomic factors. | Percentage of the population with unmet healthcare needs, waiting times for appointments | Health surveys, administrative data |
Importance of Ongoing Monitoring and Evaluation
Ongoing monitoring and evaluation are essential for:
- Tracking Progress:Regular monitoring allows policymakers and health professionals to assess the effectiveness of interventions aimed at reducing health inequalities.
- Identifying Areas for Improvement:By analyzing data over time, researchers can identify areas where disparities persist or are worsening, prompting the development of new strategies.
- Accountability:Ongoing monitoring helps ensure that resources are being allocated effectively and that interventions are making a tangible difference in reducing health inequalities.
End of Discussion: Inequalities Health
Addressing health inequalities requires a multifaceted approach that tackles the root causes of these disparities. This involves not only improving access to healthcare but also addressing broader social determinants of health, such as poverty, education, and housing. By investing in equitable policies, strengthening community engagement, and promoting individual empowerment, we can work towards a future where health is not a matter of chance but a fundamental right for all.
Commonly Asked Questions
What is the difference between health inequalities and health disparities?
Health inequalities refer to the systematic and avoidable differences in health status between different population groups, while health disparities focus on the gaps in health outcomes between specific groups, often related to race, ethnicity, or socioeconomic status.
How do health inequalities impact individuals?
Health inequalities can lead to shorter life expectancies, higher rates of chronic diseases, and reduced quality of life for individuals. They can also exacerbate existing health conditions and limit access to essential healthcare services.
What are some examples of health inequalities?
Examples include higher rates of infant mortality in low-income communities, increased risk of cardiovascular disease among certain racial groups, and disparities in access to mental health services based on gender and socioeconomic status.
What is the role of policy in addressing health inequalities?
Policy plays a crucial role in addressing health inequalities by promoting equity in access to healthcare, education, employment, and other essential resources. This includes policies aimed at reducing poverty, improving housing conditions, and ensuring equal opportunities for all.