Health coders play a crucial role in the healthcare system, ensuring accurate medical documentation and financial reimbursement. They are the unsung heroes behind the scenes, translating complex medical information into standardized codes that drive patient care and financial processes.
These dedicated professionals analyze medical records, assign codes based on standardized coding systems like ICD-10-CM and CPT, and ensure compliance with regulations. Their meticulous work helps hospitals, clinics, and insurance companies manage patient care, track outcomes, and ensure proper financial compensation.
What is a Health Coder?
Health coders are vital members of the healthcare system, playing a crucial role in the accurate and efficient management of patient health information. They translate medical diagnoses, procedures, and treatments into standardized codes, which are used for billing, research, and public health reporting.
The Role of a Health Coder
Health coders are responsible for ensuring that medical records are coded accurately and consistently, according to established coding guidelines. They use their knowledge of medical terminology, anatomy, physiology, and coding systems to interpret patient records and assign the appropriate codes.
This process is essential for accurate billing, ensuring that healthcare providers are reimbursed for their services, and for tracking patient outcomes and trends in healthcare.
Key Responsibilities and Tasks
Health coders perform a wide range of tasks, including:
- Reviewing patient medical records to identify diagnoses, procedures, and treatments.
- Assigning codes from standardized coding systems, such as the International Classification of Diseases (ICD) and Current Procedural Terminology (CPT).
- Ensuring that codes are accurate and consistent with the documentation in the patient’s medical record.
- Maintaining knowledge of coding guidelines and regulations.
- Working with other healthcare professionals, such as physicians and billing specialists.
- Performing quality control checks on coded data.
- Using specialized software programs to code medical records.
Types of Health Coding Specialties
Health coding is a diverse field with various specialties. Some common specialties include:
- Inpatient Coding:Focuses on coding records for patients admitted to hospitals.
- Outpatient Coding:Specializes in coding records for patients who receive care in physician offices, clinics, or other outpatient settings.
- Surgical Coding:Concentrates on coding surgical procedures and related services.
- Anesthesia Coding:Specializes in coding anesthesia services.
- Mental Health Coding:Focuses on coding mental health diagnoses and treatments.
The Importance of Health Coding

Health coding is a crucial component of the healthcare system, playing a vital role in patient care, financial reimbursement, and healthcare data analysis. Accurate health coding ensures that patients receive appropriate care, providers are fairly compensated, and healthcare data is reliable for research and quality improvement initiatives.
Impact on Patient Care
Accurate health coding directly impacts patient care by ensuring that medical records accurately reflect the services provided. This information helps physicians and other healthcare professionals make informed decisions about patient treatment. For instance, a correctly coded diagnosis allows healthcare providers to understand the patient’s health condition and develop an appropriate treatment plan.
In addition, accurate coding facilitates the identification of patients with specific health conditions, enabling targeted interventions and preventive measures.
Role in Financial Reimbursement
Health coding is essential for financial reimbursement in the healthcare industry. Healthcare providers submit coded medical records to insurance companies and government agencies to receive payment for services rendered. Accurate coding ensures that providers are appropriately compensated for their services, which is crucial for the financial sustainability of healthcare organizations.
Conversely, inaccurate coding can lead to underpayment or denial of claims, resulting in financial losses for providers.
Contribution to Healthcare Data Analysis and Research
Health coding provides the foundation for healthcare data analysis and research. Coded data from medical records allows researchers to identify trends, analyze patient outcomes, and develop new treatments and interventions. For example, by analyzing coded data, researchers can determine the prevalence of specific diseases, the effectiveness of different treatments, and the impact of healthcare policies.
This information is crucial for improving healthcare quality, reducing costs, and advancing medical knowledge.
Health coders play a crucial role in ensuring accurate medical billing and documentation, which is particularly important in specialized settings like a childrens mental health hospital. These facilities often require specific coding expertise to accurately reflect the complex needs of their young patients, contributing to the overall financial stability and effective treatment plans.
Health Coding Standards and Regulations

Health coding is a complex process that requires adherence to strict standards and regulations. These standards ensure accuracy, consistency, and uniformity in the coding process, which is crucial for accurate billing, reimbursement, and healthcare data analysis.
Coding Systems Used in Healthcare
The accuracy and consistency of health coding depend heavily on the use of standardized coding systems. These systems provide a common language for describing medical diagnoses, procedures, and services. Two of the most important coding systems used in the United States are:
- ICD-10-CM (International Classification of Diseases, Tenth Revision, Clinical Modification): This system is used to code diagnoses, symptoms, and reasons for patient encounters. It is a comprehensive system that includes over 14,000 codes, each representing a specific medical condition or health problem.
- CPT (Current Procedural Terminology): This system is used to code medical, surgical, and diagnostic procedures. It includes over 10,000 codes, each representing a specific procedure or service.
The Importance of Adhering to Coding Guidelines and Regulations
Coding guidelines and regulations are essential for ensuring accurate and consistent coding. They provide specific instructions on how to apply codes, interpret medical documentation, and select the most appropriate codes for each patient encounter. Adhering to these guidelines is crucial for:
- Accurate billing and reimbursement: Correct coding ensures that healthcare providers receive appropriate reimbursement for the services they provide. Incorrect coding can lead to underpayment or even denial of claims.
- Compliance with federal and state regulations: The Centers for Medicare & Medicaid Services (CMS) and other regulatory bodies have strict guidelines for coding practices. Failure to comply with these regulations can result in penalties, fines, and even legal action.
- Data integrity and analysis: Accurate coding is essential for collecting and analyzing healthcare data. This data is used for research, public health initiatives, and quality improvement programs.
Consequences of Coding Errors
Coding errors can have significant consequences for healthcare providers, patients, and the healthcare system as a whole. Some of the potential consequences include:
- Financial losses: Incorrect coding can lead to underpayment or denial of claims, resulting in financial losses for healthcare providers.
- Audits and investigations: Coding errors can trigger audits and investigations by regulatory bodies, which can be time-consuming and costly.
- Reputational damage: Coding errors can damage a healthcare provider’s reputation and erode patient trust.
- Legal liability: In some cases, coding errors can lead to legal liability, particularly if they result in patient harm.
The Health Coding Process

The health coding process is a crucial step in the medical billing and reimbursement cycle. It involves converting medical documentation into standardized codes that accurately represent the patient’s diagnosis, procedures, and services. This process ensures that healthcare providers receive appropriate reimbursement for their services and that patients are accurately classified for statistical purposes.
Data Collection
Data collection is the first step in the health coding process. It involves gathering all relevant medical documentation, including patient charts, laboratory reports, radiology images, and other pertinent records. This documentation provides the foundation for accurately coding the patient’s care.
Review and Interpretation of Medical Documentation
Once the data is collected, health coders carefully review and interpret the medical documentation. This involves understanding the patient’s medical history, current condition, and the treatments provided. They must be able to identify the key elements of the patient’s care and accurately translate them into the appropriate codes.
Coding Software and Resources
Health coders rely on coding software and resources to assist them in their work. These tools include:
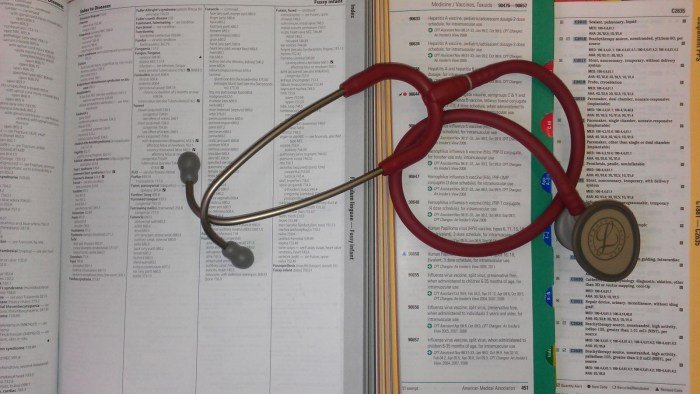
- Coding manuals: These manuals provide detailed information on the various codes used in the healthcare industry. The most commonly used manuals include the ICD-10-CM (International Classification of Diseases, Tenth Revision, Clinical Modification) for diagnoses and the CPT (Current Procedural Terminology) for procedures.
- Coding software: Coding software streamlines the coding process by providing tools for searching codes, assigning codes, and generating reports. These software programs often incorporate the latest coding updates and regulations.
- Online resources: Various online resources are available to health coders, such as the Centers for Medicare & Medicaid Services (CMS) website, which provides coding updates, guidelines, and educational materials.
Code Assignment
After reviewing the medical documentation and consulting coding resources, health coders assign codes to the patient’s diagnoses, procedures, and services. This process involves selecting the most accurate and specific codes that reflect the patient’s care.
Code Review and Verification
Once codes are assigned, they are reviewed and verified for accuracy and completeness. This step ensures that the codes are compliant with coding regulations and that the medical documentation supports the assigned codes.
Documentation of the Coding Process
Health coders must document their coding process, including the codes assigned, the rationale for the code selection, and any challenges encountered. This documentation serves as a record of the coding process and helps to ensure transparency and accountability.
Code Submission
The final step in the health coding process is the submission of the assigned codes to the appropriate parties, such as insurance companies or government agencies. This submission triggers the billing and reimbursement process.
Skills and Qualifications for Health Coders
To be a successful health coder, a blend of technical skills, knowledge, and soft skills is crucial. These skills allow coders to navigate complex medical information, ensure accurate billing, and maintain compliance with regulations.
Educational Requirements and Certifications
The path to becoming a certified health coder typically involves a combination of education and certification. While a high school diploma or equivalent is often the minimum requirement, pursuing a formal education significantly enhances career prospects.
- Associate’s Degree or Certificate:Many health coding programs are offered at the associate’s degree level, equipping students with a comprehensive understanding of coding principles, medical terminology, and anatomy. These programs often include hands-on training and internships, providing valuable real-world experience.
- Bachelor’s Degree:For those seeking advanced roles or management positions, a bachelor’s degree in health information management (HIM) or a related field can be beneficial. These programs delve deeper into healthcare administration, data analysis, and research, preparing graduates for leadership roles.
Certification is a vital step for health coders, demonstrating their competency and professionalism. Several organizations offer recognized certifications, including:
- American Health Information Management Association (AHIMA):AHIMA offers the Registered Health Information Technician (RHIT) and the Registered Health Information Administrator (RHIA) certifications. These credentials are highly respected in the industry and are often required for employment.
- American Academy of Professional Coders (AAPC):AAPC offers various coding certifications, including the Certified Professional Coder (CPC) and the Certified Outpatient Coder (COC). These certifications focus on specific coding specialties and can enhance career opportunities.
Essential Skills for Health Coders
Beyond formal education and certifications, health coders need a strong foundation of essential skills. These skills enable them to perform their duties effectively and contribute to the overall efficiency of healthcare organizations.
- Medical Terminology and Anatomy:A deep understanding of medical terminology and anatomy is fundamental for accurately interpreting medical records and assigning appropriate codes. This knowledge allows coders to identify diagnoses, procedures, and other medical information accurately.
- ICD-10-CM and CPT Coding Systems:Proficient use of the International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM) and the Current Procedural Terminology (CPT) coding systems is essential. These systems are the foundation of medical coding, providing a standardized language for describing diagnoses, procedures, and other medical services.
- Attention to Detail:Health coding involves meticulous attention to detail. Coders must carefully analyze medical records, identifying and interpreting even subtle variations in patient information. This meticulousness ensures accuracy in code assignment and proper billing.
- Analytical Skills:Health coders need to analyze medical records, identify relevant information, and apply coding rules to assign accurate codes. This requires strong analytical skills to decipher complex medical information and make informed coding decisions.
- Problem-Solving Skills:Coding often involves resolving ambiguities or inconsistencies in medical records. Health coders need to identify and resolve these issues, using their knowledge of coding guidelines and their analytical skills to ensure accurate code assignment.
- Communication Skills:Effective communication is vital for health coders. They need to communicate clearly with physicians, other healthcare professionals, and billing departments, ensuring everyone understands the coding process and its implications.
- Computer Skills:Health coders work extensively with computer systems, including electronic health records (EHRs) and coding software. Proficient computer skills, including data entry, software navigation, and basic troubleshooting, are essential.
Career Paths and Opportunities: Health Coder

The field of health coding offers a stable and rewarding career path with diverse opportunities for growth and advancement. Health coders play a crucial role in the healthcare system, ensuring accurate medical billing and claims processing, which ultimately impacts patient care and financial stability of healthcare providers.
Job Outlook and Career Progression
The job outlook for health coders is positive, with projected growth in the coming years. The Bureau of Labor Statistics (BLS) predicts a 13% increase in employment for medical records and health information technicians, which includes health coders, from 2021 to 2031, faster than the average for all occupations.
This growth is driven by several factors, including the increasing demand for healthcare services, the implementation of electronic health records (EHRs), and the growing emphasis on data analytics in healthcare.
- Entry-Level Positions:Health coders typically start their careers as coding specialists or assistants, gaining experience in coding medical records and working under the supervision of senior coders.
- Advancement Opportunities:With experience and certifications, health coders can progress to roles such as lead coder, coding supervisor, or coding manager. These roles involve overseeing coding teams, ensuring coding accuracy, and implementing coding policies.
- Specialization:Health coders can specialize in specific areas of coding, such as inpatient coding, outpatient coding, or coding for specific medical specialties. This specialization can lead to higher salaries and more specialized job opportunities.
Work Environments
Health coders can find employment in various healthcare settings, each offering unique experiences and challenges.
- Hospitals:Hospitals are the largest employers of health coders, offering a wide range of coding opportunities across different departments, such as inpatient, outpatient, emergency room, and surgery.
- Clinics:Clinics, including physician practices and specialty clinics, also employ health coders to handle coding for patient encounters and billing. The workload in clinics is often smaller than in hospitals, providing a more intimate work environment.
- Insurance Companies:Insurance companies employ health coders to review medical claims, ensuring that they are coded accurately and meet the requirements for reimbursement. This role requires a strong understanding of insurance policies and coding regulations.
- Software and Consulting Firms:With the rise of EHRs and healthcare data analytics, software and consulting firms are increasingly hiring health coders to develop and implement coding solutions and provide expert advice to healthcare providers.
Emerging Trends and Future Opportunities
The field of health coding is constantly evolving, driven by technological advancements and changing healthcare regulations.
- Artificial Intelligence (AI) and Machine Learning (ML):AI and ML are being increasingly used in health coding to automate tasks, improve coding accuracy, and identify potential errors. Health coders with expertise in these technologies will be in high demand.
- Data Analytics:As healthcare data becomes more complex, health coders with data analytics skills will be needed to analyze coding data, identify trends, and improve coding practices.
- Remote Work:The rise of remote work has opened up new opportunities for health coders, allowing them to work from home or other remote locations.
Challenges and Trends in Health Coding
Health coding, a vital aspect of healthcare administration, is constantly evolving to adapt to changing technologies and regulations. This dynamic field presents unique challenges and exciting trends that shape the future of health coding professionals.
Health coders play a crucial role in ensuring accurate medical billing and documentation, a process that is particularly important in settings like a whole family health center , where diverse patient needs require meticulous record keeping. By assigning specific codes to diagnoses and procedures, health coders help streamline patient care and ensure proper reimbursement for the services provided.
Coding Complexity and Regulatory Changes
Health coding involves deciphering complex medical terminology and applying precise codes to patient records. This task is further complicated by the frequent updates and changes to coding guidelines, such as the International Classification of Diseases (ICD) and Current Procedural Terminology (CPT) manuals.
For example, the implementation of ICD-10-CM in 2015 brought about a significant increase in the number of codes, requiring health coders to adapt to a more granular system.
This complexity demands ongoing professional development and continuous learning to stay current with evolving coding standards and regulations.
Health coders play a vital role in ensuring accurate medical billing, and staying active is crucial for overall well-being. If you’re a health coder in Boca Raton, consider checking out the Boca Raton Health Club for a great workout spot.
A healthy lifestyle can lead to better mental and physical health, which can also benefit your performance as a health coder.
The Rise of Electronic Health Records (EHRs)
The widespread adoption of electronic health records (EHRs) has transformed the healthcare landscape, impacting health coding in various ways. EHRs have automated many coding processes, reducing manual effort and improving efficiency.
However, EHR systems can also introduce new challenges, such as data entry errors and inconsistencies, which require careful attention and validation by health coders.
EHRs have also led to an increased demand for skilled health coders who can navigate these systems effectively and ensure data accuracy.
The Impact of Artificial Intelligence (AI) and Machine Learning
Artificial intelligence (AI) and machine learning (ML) are emerging technologies that are transforming various industries, including healthcare. In health coding, AI and ML have the potential to automate tasks, improve accuracy, and enhance efficiency.
AI-powered tools can analyze large datasets of patient records, identify patterns, and suggest appropriate codes, potentially reducing the workload for human coders.
While AI and ML hold immense promise, it’s important to recognize that they are not a complete replacement for human expertise. Health coders will continue to play a critical role in ensuring the accuracy and integrity of coded data.
Final Wrap-Up

The field of health coding is constantly evolving, driven by advancements in technology, regulations, and healthcare practices. As the healthcare landscape shifts, health coders must adapt and stay abreast of new developments to maintain their value and contribute to the overall efficiency and effectiveness of the healthcare system.
FAQ Guide
What are the different types of health coding specialties?
Health coding specialties include inpatient coding, outpatient coding, surgical coding, and specialty coding (e.g., oncology, cardiology).
How do I become a certified health coder?
You typically need an associate’s degree in health information management or a related field, followed by passing a certification exam offered by organizations like the American Health Information Management Association (AHIMA).
What are the salary expectations for health coders?
Salaries vary based on experience, location, and employer, but generally range from $40,000 to $70,000 per year.