Independent health systems are a crucial component of the healthcare landscape, offering a unique model of care that often prioritizes community needs and patient-centered approaches. Unlike large, integrated delivery networks (IDNs), independent health systems typically operate autonomously, often with a strong emphasis on local governance and physician leadership.
This autonomy allows them to respond more readily to the specific health challenges and preferences of their communities.
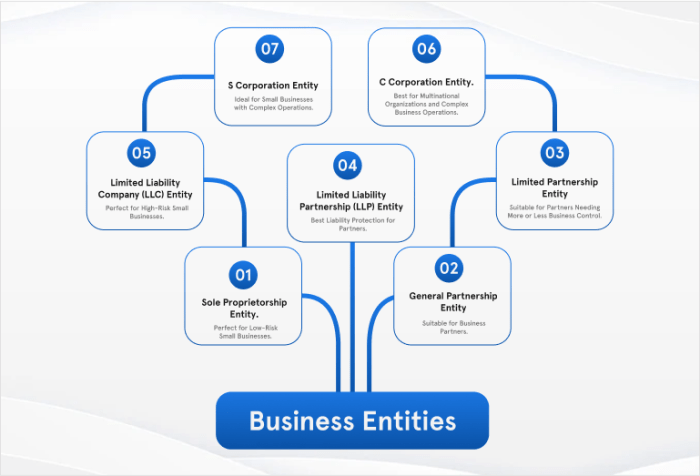
These systems are characterized by a diverse range of organizational structures, financial models, and operational strategies. Some independent health systems are physician-owned and operated, while others are non-profit or for-profit entities. The financial sustainability of these systems can be influenced by factors such as patient volume, payer mix, and cost containment strategies.
Despite the challenges of navigating a competitive healthcare market, independent health systems play a vital role in providing access to care, improving patient outcomes, and addressing community health needs.
Definition and Characteristics
Independent health systems are healthcare organizations that operate autonomously, often encompassing multiple facilities like hospitals, clinics, and physician practices. They are distinct from integrated delivery networks (IDNs) and hospital systems in terms of ownership, governance, and operational structure.
Ownership and Governance
Independent health systems are typically owned and governed by a board of directors, which may include community members, physicians, and other stakeholders. This structure allows for a greater degree of local control and responsiveness to community needs.
Operational Structure
Independent health systems typically have a decentralized operational structure, with individual facilities maintaining a high level of autonomy. This allows for greater flexibility and adaptability to local market conditions.
Benefits of Independent Health Systems
- Community Focus:Independent health systems are often deeply rooted in their communities, fostering strong relationships with local residents and providers. This can lead to a greater emphasis on community health initiatives and outreach programs.
- Flexibility and Adaptability:The decentralized structure of independent health systems allows them to respond more quickly to changes in the healthcare landscape, such as shifts in patient demographics or technological advancements.
- Local Control:Independent health systems have a greater degree of control over their operations, enabling them to tailor their services to the specific needs of their communities.
Challenges of Independent Health Systems
- Financial Sustainability:Independent health systems may face challenges in competing with larger, integrated healthcare organizations, which often have greater bargaining power with insurers and suppliers.
- Access to Resources:Smaller, independent health systems may have limited access to resources, such as advanced technology or specialized medical expertise, compared to larger systems.
- Mergers and Acquisitions:In a competitive healthcare market, independent health systems may face pressure to merge or be acquired by larger organizations to achieve economies of scale and enhance their financial stability.
Organizational Structure and Governance: Independent Health Systems
Independent health systems, operating outside the confines of larger networks, often adopt unique organizational structures and governance models to cater to their specific needs and objectives. These structures play a crucial role in shaping the system’s decision-making processes, resource allocation, and overall direction.
Organizational Structure
The organizational structure of an independent health system typically involves a hierarchical arrangement, with a board of directors at the apex, followed by administrative leadership and medical staff.
- Board of Directors: The board of directors, typically composed of community leaders, healthcare professionals, and financial experts, provides strategic oversight and guidance to the health system. They establish policies, approve budgets, and appoint senior leadership. Their primary focus is on ensuring the long-term viability and mission alignment of the system.
- Administrative Leadership: The administrative leadership team, led by a chief executive officer (CEO), is responsible for the day-to-day operations of the health system. This team manages finances, human resources, facilities, and other essential functions. They work closely with the board of directors to implement strategic initiatives and ensure efficient operations.
- Medical Staff: The medical staff, comprised of physicians, nurses, and other healthcare professionals, provides direct patient care. Their role involves clinical decision-making, patient education, and collaboration with administrative leadership to improve quality of care. The medical staff often has a significant voice in governance through committees and councils, ensuring their clinical expertise is integrated into decision-making processes.
Independent health systems offer a unique perspective on patient care, often prioritizing personalized attention and community engagement. This commitment to individual well-being extends beyond medical services, encompassing a holistic approach that recognizes the importance of self-care. For example, a thriving aspect of this philosophy is the emphasis on personal appearance, as reflected in the numerous beauty salons in Lawrence, KS.
These salons provide a space for individuals to enhance their appearance and boost their confidence, contributing to overall well-being. Ultimately, independent health systems strive to create a supportive environment that empowers individuals to take control of their health and wellness, both physically and mentally.
Governance Models
Independent health systems can adopt various governance models, each with its own strengths and challenges. Some common models include:
- Physician-Led Governance: In this model, physicians hold a majority of the board seats, giving them significant influence over the system’s strategic direction and clinical decision-making. This model is often favored for its emphasis on patient care and clinical quality but can lead to challenges in managing administrative and financial aspects.
- Community-Based Governance: Community-based governance emphasizes the involvement of local stakeholders, such as community leaders, business representatives, and patients, in decision-making. This model promotes transparency and accountability to the community but may require navigating diverse perspectives and interests.
- For-Profit Entities: Some independent health systems operate as for-profit entities, aiming to generate profits for their shareholders. This model can incentivize innovation and efficiency but may prioritize financial returns over community health needs.
Examples of Successful Independent Health Systems
Several independent health systems have achieved success through their unique governance structures.
- The Cleveland Clinic, a renowned non-profit academic medical center, is known for its physician-led governance model. The clinic’s board of directors is composed primarily of physicians, who actively participate in strategic planning and clinical decision-making. This structure has fostered a culture of clinical excellence and innovation, contributing to the clinic’s reputation as a leading healthcare provider.
Independent health systems offer a variety of services, often catering to specific needs. While their focus may differ from a company like ulta beauty hq , which specializes in beauty products, both aim to provide a positive experience for their customers.
Ultimately, independent health systems strive to empower individuals to take control of their well-being, just as Ulta Beauty empowers customers to express their personal style.
- Intermountain Healthcare, a large non-profit system based in Utah, has successfully implemented a community-based governance model. The system’s board includes representatives from various communities within its service area, ensuring diverse perspectives are considered in decision-making. This approach has fostered trust and engagement with the local communities, strengthening the system’s commitment to serving the needs of its patients.
Financial Sustainability and Operations
Independent health systems operate within a complex and dynamic healthcare landscape, where financial stability is paramount for delivering quality patient care and achieving long-term sustainability. Understanding the financial models, revenue streams, and operational strategies of these systems is crucial to navigating the challenges and opportunities they face.
Financial Models and Revenue Streams
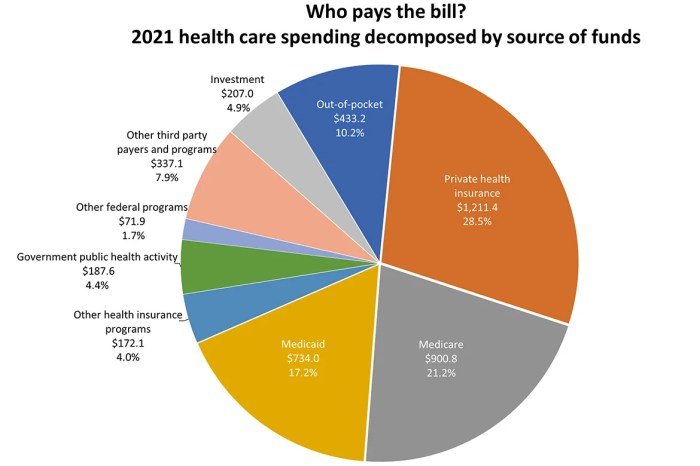
The financial sustainability of independent health systems relies on a diverse mix of revenue streams and cost containment strategies. Key factors influencing their financial performance include patient volume, payer mix, and the ability to manage expenses effectively.
- Patient Volume:Independent health systems generate revenue primarily from patient services, with volume playing a critical role in profitability. Higher patient volumes can translate into increased revenue, but it’s essential to balance volume with the provision of high-quality care. Effective marketing, community outreach, and strong relationships with referring physicians are crucial for attracting patients.
- Payer Mix:The mix of payers, such as commercial insurance, Medicare, Medicaid, and self-pay patients, significantly impacts revenue. Negotiating favorable contracts with commercial insurers and managing the complexities of government programs are essential for financial stability. Independent health systems often focus on building a diverse payer mix to mitigate the risks associated with relying heavily on any single payer source.
- Cost Containment Strategies:In today’s competitive healthcare market, independent health systems must actively manage costs to maintain profitability. Strategies include:
- Efficient Operations:Streamlining administrative processes, leveraging technology for automation, and optimizing supply chain management can reduce operational expenses.
- Value-Based Care:Shifting from fee-for-service models to value-based care arrangements, which reward providers for quality outcomes rather than volume, can improve financial performance by incentivizing cost-effective care delivery.
- Clinical Integration:Integrating clinical services and care coordination can improve efficiency, reduce duplication of services, and enhance patient outcomes.
Challenges to Financial Stability
Independent health systems face a range of challenges in maintaining financial stability, including:
- Competition:The healthcare market is increasingly competitive, with large hospital systems and integrated delivery networks posing significant challenges to independent systems. Independent systems often struggle to compete on price and scale, particularly in areas with limited market share.
- Changing Payment Models:The transition from fee-for-service to value-based care models requires independent systems to adapt their operational models and clinical practices to succeed. Navigating complex reimbursement structures and demonstrating value-based performance can be challenging.
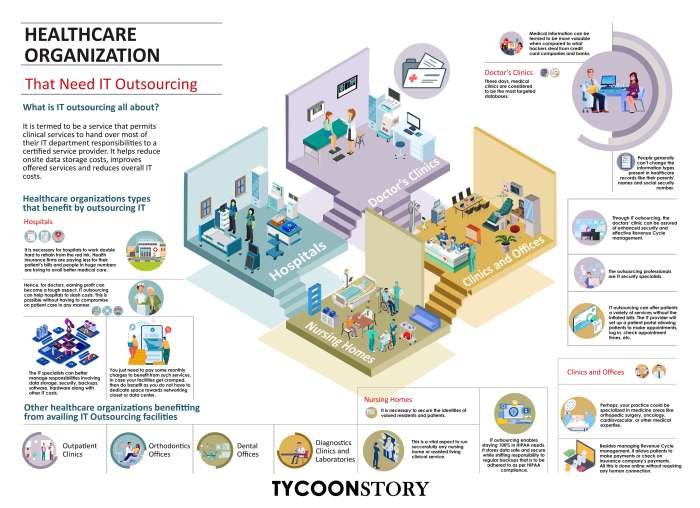
- Technology Investments:Maintaining a competitive edge in technology, including electronic health records (EHRs), data analytics, and telehealth platforms, is essential for efficient operations and patient care. Investing in technology can be costly, requiring independent systems to carefully prioritize investments and secure funding.
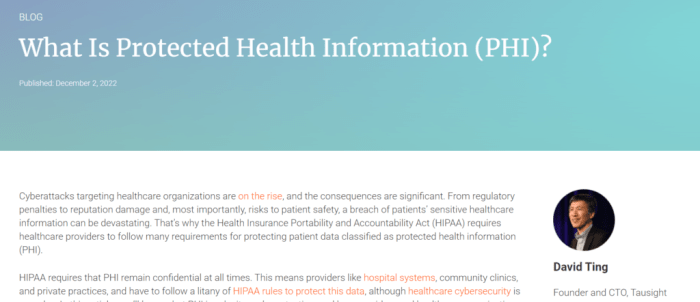
- Regulatory Environment:The healthcare industry is subject to a complex web of regulations, which can impact financial performance. Independent systems must comply with changing regulations, such as those related to privacy, data security, and billing practices, while navigating the complexities of government programs.
Operational Aspects
Independent health systems operate with a focus on delivering high-quality patient care while maintaining financial sustainability. Key operational aspects include:
| Operational Aspect | Description |
|---|---|
| Patient Care Delivery | Independent health systems typically offer a comprehensive range of services, including primary care, specialty care, emergency services, and outpatient services. They strive to provide patient-centered care, emphasizing communication, coordination, and personalized treatment plans. |
| Technology Adoption | Independent systems are increasingly adopting technology to enhance patient care, improve operational efficiency, and manage costs. This includes implementing EHRs, telehealth platforms, and data analytics tools to streamline processes, improve patient engagement, and support decision-making. |
| Community Engagement | Independent health systems often play a vital role in their communities, providing access to care for underserved populations and participating in community health initiatives. They may offer outreach programs, health education, and community partnerships to address local health needs. |
Impact on Patient Care and Community Health
Independent health systems play a crucial role in shaping the healthcare landscape, influencing patient care quality, access, and affordability, while actively engaging in addressing community health needs and promoting health equity. This section delves into the multifaceted impact of these systems on both individual patients and the broader community.
Impact on Patient Care Quality
Independent health systems often prioritize patient-centered care, fostering a personalized approach to treatment. Their smaller size and local focus enable them to cultivate strong patient-provider relationships, leading to improved communication, trust, and adherence to treatment plans. Studies have shown that patients treated at independent hospitals often experience higher satisfaction scores and better outcomes.
Impact on Patient Access
Independent health systems play a significant role in ensuring access to healthcare, particularly in underserved areas. Their presence in rural and suburban communities, often lacking large hospital networks, provides essential medical services to populations who might otherwise face significant barriers to care.
They also frequently operate community health centers and clinics, expanding outreach and accessibility for vulnerable populations.
Impact on Patient Affordability
Independent health systems can contribute to affordability in healthcare by offering competitive pricing and negotiating lower costs with insurance providers. Their independence allows them to tailor their services and pricing strategies to meet the specific needs of their communities. They often focus on providing high-quality care at a lower cost, making healthcare more accessible to a broader range of patients.
Role in Addressing Community Health Needs
Independent health systems are actively involved in addressing community health needs, promoting health equity, and improving overall well-being. They often collaborate with local organizations, community leaders, and public health agencies to identify and address health disparities, implement preventive health programs, and provide health education resources.
Independent health systems often face the challenge of coordinating care across multiple providers and locations. To streamline communication and collaboration, many are turning to online portals like the IU Health Teams Portal. This platform provides a centralized hub for secure messaging, scheduling, and patient information, helping to improve efficiency and enhance the overall patient experience within independent health systems.
Examples of Innovative Initiatives, Independent health systems
Independent health systems are at the forefront of innovation in healthcare, implementing initiatives to improve patient outcomes and community well-being. Examples include:
- Developing telehealth programs to expand access to specialty care in rural areas.
- Partnering with local schools to provide health education and screenings for children.
- Launching community health fairs to promote healthy lifestyles and disease prevention.
- Establishing mobile clinics to provide healthcare services to homeless populations and other vulnerable groups.
- Implementing patient navigation programs to guide patients through complex healthcare systems and ensure access to necessary resources.
Trends and Future of Independent Health Systems

Independent health systems are facing a dynamic landscape marked by significant trends and challenges that are shaping their future trajectory. These systems are navigating a complex environment characterized by consolidation, technological advancements, and evolving regulatory landscapes. This section delves into these trends and explores potential future directions for independent health systems.
Consolidation and Competition
The healthcare industry is experiencing a wave of consolidation, with large hospital systems and health insurance companies acquiring smaller, independent providers. This trend presents both opportunities and challenges for independent health systems. While consolidation can offer economies of scale and access to resources, it also increases competition and can potentially limit patient choice.
Independent health systems are increasingly finding themselves competing with larger, integrated systems that offer a wider range of services and have greater bargaining power with payers.
Last Point
The future of independent health systems is intertwined with the broader evolution of healthcare. As technology advances and the healthcare landscape continues to transform, independent health systems will need to adapt and innovate to remain competitive. They may explore partnerships, mergers, or specialized service offerings to enhance their capabilities and meet the evolving needs of their communities.
By embracing innovation and maintaining a focus on patient-centered care, independent health systems can continue to be a vital force in delivering high-quality healthcare and improving health outcomes for all.
Helpful Answers
What are the advantages of independent health systems?
Independent health systems often offer a more personalized and responsive approach to patient care. They may also have stronger ties to their communities and be more attuned to local health needs.
What are the challenges faced by independent health systems?
Independent health systems face challenges such as negotiating with large insurers, managing financial stability in a competitive market, and keeping up with technological advancements.
How do independent health systems contribute to community health?
Independent health systems often play a significant role in addressing health disparities, providing access to care for underserved populations, and promoting health equity within their communities.