Inequalities health – Health Inequalities: A Global Challenge, explores the disparities in health outcomes across different populations and geographical regions. It delves into the complex interplay of social, economic, and environmental factors that contribute to these inequalities, revealing how they impact individuals throughout their lifespan.
This exploration highlights the role of healthcare systems in either exacerbating or mitigating these disparities, examining the impact of access, quality of care, and financing on health outcomes. Ultimately, the discussion focuses on strategies for promoting health equity and reducing health inequalities, sharing best practices and policy recommendations from around the world.
Definition and Scope of Health Inequalities: Inequalities Health

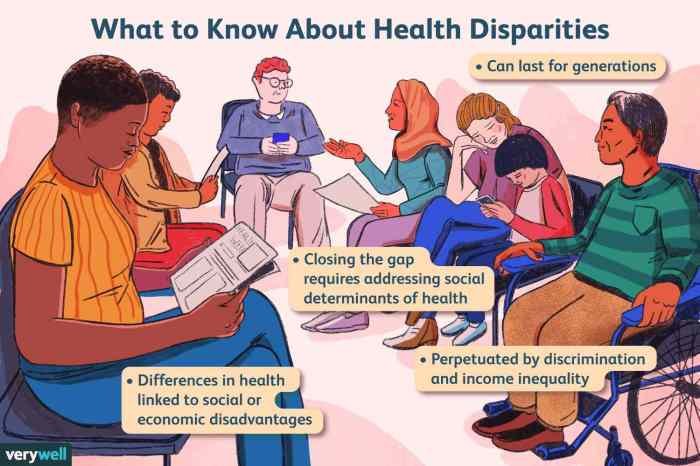
Health inequalities refer to the avoidable and unfair differences in health status between different population groups. These differences are often rooted in social, economic, and environmental factors that create barriers to accessing healthcare and achieving optimal health outcomes.
Distinguishing Health Inequalities from Health Disparities
Health inequalities and health disparities are often used interchangeably, but they have distinct meanings. Health disparities refer to any difference in health status between population groups. These differences may be due to factors such as genetics, lifestyle choices, or access to healthcare.
However, health inequalities specifically focus on the unfair and avoidable differences in health status that are rooted in social, economic, and environmental factors.
Social, Economic, and Environmental Factors Contributing to Health Inequalities
Several factors contribute to health inequalities, and they often interact in complex ways. These factors can be broadly categorized into social, economic, and environmental categories.
Inequalities in health access often stem from socioeconomic disparities. One way to address this is by promoting affordable fitness options, such as Crunch Fitness Allen , which offers a range of membership plans. By making fitness accessible to a wider population, we can work towards a more equitable healthcare system.
Social Factors
Social factors that contribute to health inequalities include:
- Socioeconomic status:Individuals with lower socioeconomic status are more likely to experience poor health outcomes due to limited access to quality healthcare, nutritious food, safe housing, and education.
- Education level:Education plays a crucial role in health outcomes. Individuals with higher levels of education tend to have better health knowledge, access to healthcare, and employment opportunities, leading to improved health status.
- Social isolation and loneliness:Social isolation and loneliness are associated with increased risk of chronic diseases and premature mortality.
- Discrimination:Discrimination based on race, ethnicity, gender, sexual orientation, or disability can create barriers to healthcare access and contribute to health inequalities.
Economic Factors
Economic factors that contribute to health inequalities include:
- Income inequality:High levels of income inequality within a society can lead to greater health inequalities.
- Unemployment:Unemployment is linked to poor health outcomes due to financial insecurity, stress, and lack of access to healthcare.
- Access to affordable housing:Individuals living in overcrowded or substandard housing are at increased risk of health problems.
Environmental Factors
Environmental factors that contribute to health inequalities include:
- Air pollution:Exposure to air pollution is linked to respiratory problems, cardiovascular disease, and other health issues.
- Water quality:Access to clean and safe drinking water is essential for health.
- Noise pollution:Prolonged exposure to noise pollution can lead to stress, sleep disturbances, and cardiovascular problems.
Examples of Health Inequalities Across Different Populations and Geographical Regions
Health inequalities are observed across various populations and geographical regions. Some examples include:
- Race and ethnicity:In many countries, racial and ethnic minorities experience higher rates of chronic diseases and premature mortality compared to their white counterparts. For example, in the United States, African Americans have higher rates of heart disease, stroke, diabetes, and cancer compared to white Americans.
- Gender:Women and girls face unique health challenges, including higher rates of certain diseases and limited access to healthcare in some regions.
- Geographical location:People living in rural areas or marginalized communities often have limited access to healthcare services, leading to poorer health outcomes.
- Income level:Individuals with lower incomes are more likely to experience poor health outcomes due to limited access to healthcare, nutritious food, and safe housing.
Social Determinants of Health Inequalities

The social determinants of health are the non-medical factors that influence health outcomes. These factors include socioeconomic status, education, employment, housing, food security, access to healthcare, social isolation, discrimination, and stress. They play a significant role in shaping health inequalities, creating disparities in health status across different population groups.
Socioeconomic Status, Education, and Employment
Socioeconomic status (SES) is a major determinant of health, encompassing income, wealth, education, and occupation. Lower SES is associated with poorer health outcomes, including higher rates of chronic diseases, premature mortality, and disability. Education plays a crucial role in determining SES and health.
Higher education levels are linked to better health knowledge, healthier behaviors, and greater access to resources. Employment provides income, social support, and a sense of purpose, all of which contribute to better health. However, unemployment, precarious employment, and occupational hazards can negatively impact health.
Housing, Food Security, and Access to Healthcare
Housing is essential for health, providing shelter, safety, and a stable environment. Inadequate housing, including homelessness, overcrowding, and exposure to environmental hazards, can lead to physical and mental health problems. Food security, the reliable access to sufficient, safe, and nutritious food, is crucial for health.
Food insecurity, characterized by limited access to food, can lead to malnutrition, chronic diseases, and poor overall health. Access to healthcare is fundamental for maintaining health and preventing disease. Barriers to healthcare access, such as cost, distance, and lack of insurance, can exacerbate health inequalities.
Social Isolation, Discrimination, and Stress
Social isolation, characterized by limited social connections and support, can negatively impact mental and physical health. Discrimination based on factors such as race, ethnicity, gender, sexual orientation, and disability can lead to stress, anxiety, and poor health outcomes. Chronic stress, caused by factors such as poverty, discrimination, and social isolation, can have a detrimental impact on health, leading to chronic diseases and premature mortality.
Health Inequalities Across the Lifespan

Health inequalities are not confined to a specific age group but rather manifest throughout the lifespan, with distinct challenges and vulnerabilities emerging at each stage. Understanding these inequalities is crucial for developing targeted interventions and promoting equitable health outcomes for all.
Health Inequalities in Childhood
Childhood is a critical period for establishing health foundations. Children from disadvantaged backgrounds are more likely to experience health inequalities, impacting their development and well-being.
- Higher rates of chronic diseases:Children from low-income families are more susceptible to chronic diseases like asthma, obesity, and diabetes due to factors like poor nutrition, limited access to healthcare, and exposure to environmental hazards. For example, a study by the CDC found that children living in poverty are more likely to have asthma than those from higher-income families.
- Developmental delays:Limited access to early childhood education and development programs can contribute to cognitive and social-emotional delays, impacting a child’s future educational and economic opportunities.
- Mental health issues:Children from disadvantaged backgrounds are at increased risk for mental health problems like anxiety and depression due to stressors like poverty, family instability, and exposure to violence.
Health Inequalities in Adolescence
Adolescence is a period of significant physical and emotional changes, making it a vulnerable time for health inequalities to emerge or worsen.
Inequalities in health care can manifest in various ways, from access to quality services to disparities in treatment outcomes. While Florida boasts a vibrant culture and stunning natural beauty, as showcased on this website , it’s crucial to acknowledge that these disparities persist and must be addressed to ensure equitable healthcare for all Floridians.
- Increased risk-taking behaviors:Adolescents from disadvantaged backgrounds may engage in risk-taking behaviors like substance use and unprotected sex due to factors like peer pressure, lack of access to support services, and feelings of hopelessness.
- Mental health challenges:Adolescence is a time of increased vulnerability to mental health issues like depression, anxiety, and eating disorders. These challenges can be exacerbated by factors like poverty, discrimination, and social isolation.
- Limited access to healthcare:Adolescents from disadvantaged backgrounds may have limited access to healthcare due to financial constraints, lack of insurance, or transportation barriers.
Health Inequalities in Adulthood
Adulthood is a time when health inequalities can have a significant impact on individuals’ lives, affecting their employment, relationships, and overall well-being.
- Chronic diseases:Adults from disadvantaged backgrounds are more likely to develop chronic diseases like heart disease, stroke, and cancer due to factors like poor diet, lack of physical activity, and exposure to environmental toxins.
- Mental health conditions:Adults from disadvantaged backgrounds are at increased risk for mental health conditions like depression, anxiety, and substance abuse.
- Limited access to healthcare:Adults from disadvantaged backgrounds may have limited access to healthcare due to factors like lack of insurance, high healthcare costs, and limited availability of services in their communities.
Health Inequalities in Old Age
Old age is a time when health inequalities can have a profound impact on individuals’ quality of life and longevity.
- Increased risk of chronic diseases:Older adults from disadvantaged backgrounds are more likely to experience chronic diseases like dementia, heart disease, and stroke due to a lifetime of exposure to health risks and limited access to healthcare.
- Functional limitations:Older adults from disadvantaged backgrounds may experience more functional limitations, such as difficulty with mobility and daily activities, due to factors like poor health, lack of access to assistive devices, and social isolation.
- Social isolation:Older adults from disadvantaged backgrounds are more likely to experience social isolation, which can negatively impact their mental and physical health.
Health Systems and Inequalities
Healthcare systems play a crucial role in shaping health outcomes, and their impact on health inequalities is undeniable. They can either exacerbate existing disparities or act as a force for positive change.
Access to Healthcare
Access to healthcare is a fundamental determinant of health. When access is limited, individuals may be unable to receive essential preventive care, timely diagnosis, or necessary treatment. This can lead to poorer health outcomes and exacerbate existing inequalities.
- Financial Barriers:High healthcare costs, lack of health insurance, and limited financial resources can restrict access to care, especially for vulnerable populations. For instance, individuals living in poverty may face challenges affording essential medications, medical procedures, or even basic healthcare visits.
- Geographic Barriers:Limited access to healthcare providers, especially in rural or underserved areas, can pose significant barriers to care. Long travel distances, limited transportation options, and the lack of available specialists can hinder access to essential services.
- Social Barriers:Discrimination, language barriers, and cultural differences can create obstacles to accessing healthcare. For example, individuals from marginalized communities may face bias from healthcare providers, leading to mistrust and reduced utilization of services.
Quality of Care
The quality of healthcare received is equally important. Disparities in the quality of care can lead to unequal health outcomes, even when access to services is similar.
- Bias and Discrimination:Implicit bias and discrimination within the healthcare system can lead to disparities in diagnosis, treatment, and referral patterns. For example, research has shown that Black patients are less likely to receive pain medication compared to White patients with similar symptoms.
- Cultural Competency:Lack of cultural competency among healthcare providers can hinder effective communication and understanding of patients’ needs, leading to misdiagnosis or inappropriate treatment. For instance, culturally sensitive approaches are crucial when addressing health concerns that are specific to certain ethnic groups or cultural backgrounds.
- Access to Specialized Care:Inequalities in access to specialized care, such as mental health services, can have a significant impact on health outcomes. Individuals from disadvantaged backgrounds may face longer wait times for appointments, limited access to specialists, or a lack of culturally appropriate care.
Healthcare Financing
Healthcare financing systems can also contribute to health inequalities. Unequal access to financial resources for healthcare can lead to disparities in health outcomes.
- Private Insurance:Private health insurance coverage is often linked to employment, which can create inequalities for individuals who are unemployed, underemployed, or work in sectors with limited benefits. Furthermore, the cost of private insurance can be prohibitive for lower-income households.
Health inequalities are a complex issue, often rooted in socioeconomic factors. Access to quality fitness facilities can play a role in addressing these disparities, and finding a gym that suits your needs is crucial. If you’re looking for a gym near you, check out edge fitness near me for options in your area.
Ultimately, improving access to affordable and accessible fitness programs can be a key step towards promoting health equity for all.
- Public Insurance:Public insurance programs, such as Medicaid, provide essential healthcare coverage for low-income individuals and families. However, these programs often face funding constraints and administrative challenges, which can impact the quality and accessibility of services.
- Cost-Sharing:Cost-sharing mechanisms, such as deductibles and co-pays, can create financial barriers for individuals with limited resources, leading to delayed or forgone care.
Addressing Health Inequalities
Addressing health inequalities is a complex and multifaceted challenge that requires a multi-sectoral approach. It necessitates a commitment to promoting health equity, ensuring that everyone has a fair and just opportunity to achieve their full health potential, regardless of their social position, economic status, or other factors.
Strategies for Promoting Health Equity, Inequalities health
Strategies for promoting health equity and reducing health inequalities are diverse and can be implemented at various levels, from individual behavior change to large-scale policy interventions.
- Social Determinants of Health:Addressing the root causes of health inequalities requires focusing on the social determinants of health. This involves tackling poverty, improving education and employment opportunities, ensuring access to safe and affordable housing, and promoting healthy living conditions.
- Health Systems:Health systems must be designed to be equitable and accessible to all. This includes ensuring that everyone has access to quality healthcare, regardless of their ability to pay. It also involves addressing disparities in access to healthcare services, particularly for vulnerable populations.
- Community-Based Interventions:Community-based interventions can play a vital role in promoting health equity. These interventions often involve working with local communities to identify and address their specific health needs. Examples include community health programs, health education initiatives, and support groups.
- Policy Changes:Policy changes can be instrumental in reducing health inequalities. This includes policies aimed at reducing poverty, improving access to education and employment, and promoting healthy living conditions.
Best Practices and Successful Interventions
Several countries and organizations have implemented successful interventions to address health inequalities. These interventions often involve a combination of strategies, including:
- Universal Health Coverage (UHC):Countries like Thailand and Rwanda have implemented universal health coverage programs, providing access to quality healthcare for all citizens, regardless of their income.
- Community Health Workers (CHWs):CHWs are trained community members who provide health education, screening, and referral services in underserved communities. They have been successful in improving access to healthcare in countries like India and South Africa.
- Early Childhood Development Programs:Programs that focus on early childhood development, such as early childhood education and nutrition interventions, can help to reduce health inequalities by providing children with a strong foundation for health and well-being.
- Multi-sectoral Collaborations:Effective interventions often involve partnerships between different sectors, including health, education, social welfare, and housing. This allows for a more comprehensive and holistic approach to addressing health inequalities.
Key Policy Recommendations
A range of policy recommendations can help to address health inequalities. These recommendations should be tailored to the specific context and needs of each country or region.
| Policy Area | Key Recommendations |
|---|---|
| Social Determinants of Health |
|
| Health Systems |
|
| Community-Based Interventions |
|
| Policy Changes |
|
Final Review
By understanding the root causes of health inequalities and implementing effective policies, we can work towards a future where everyone has the opportunity to live a long and healthy life. This journey requires a collective effort from governments, healthcare providers, communities, and individuals to create a more just and equitable society.
Frequently Asked Questions
What are the key policy recommendations for addressing health inequalities?
Policy recommendations include: expanding access to quality healthcare, addressing socioeconomic disparities, promoting health education, investing in community-based programs, and addressing environmental factors that contribute to health inequalities.
How can individuals contribute to reducing health inequalities?
Individuals can contribute by advocating for policy changes, supporting community organizations, promoting health literacy, and engaging in healthy behaviors.