Mental health examination templates are essential tools for mental health professionals, providing a structured framework for comprehensive assessments. These templates guide clinicians in gathering crucial information about a patient’s mental and physical health, history, and current concerns. They facilitate a thorough evaluation, enabling accurate diagnoses and effective treatment planning.
The use of mental health examination templates promotes consistency in assessments, ensuring that all relevant information is collected and considered. This standardized approach contributes to improved patient care, allowing for more informed decision-making and a greater likelihood of positive outcomes.
Importance of Mental Health Examinations
Mental health examinations are essential for maintaining overall well-being. Just as we schedule regular physical checkups, prioritizing mental health assessments is equally crucial. These examinations offer a valuable opportunity to identify potential mental health concerns early on, allowing for timely intervention and improving the chances of a positive outcome.
Benefits of Early Detection and Intervention
Early detection and intervention in mental health issues are vital for promoting recovery and improving quality of life. Regular mental health assessments can help identify warning signs, enabling individuals to seek professional help before symptoms worsen. This early intervention can prevent the escalation of mental health conditions, minimizing the impact on an individual’s life.
- Reduced severity of symptoms:Early intervention can significantly reduce the severity of mental health symptoms, making them more manageable and improving the chances of a full recovery. For example, individuals with anxiety disorders who receive timely treatment may experience a reduction in the frequency and intensity of their anxiety episodes, leading to a more fulfilling life.
- Improved treatment outcomes:Early intervention often leads to more effective treatment outcomes. Individuals who seek help at the onset of mental health concerns are more likely to respond positively to therapy and medication, experiencing a faster and more sustained recovery.
- Reduced risk of complications:Mental health conditions can have significant consequences for physical health, leading to chronic conditions such as heart disease, diabetes, and obesity. Early intervention can reduce the risk of these complications, improving overall health and well-being.
- Enhanced coping skills:Mental health examinations can provide individuals with valuable tools and strategies for managing stress, coping with challenges, and improving their overall mental well-being. This can empower individuals to navigate life’s difficulties with greater resilience and confidence.
Contributions to Overall Well-being
Mental health examinations contribute to overall well-being by addressing the multifaceted aspects of mental health. These assessments can identify underlying factors that may be impacting an individual’s mental health, such as stress, trauma, or relationship issues. By addressing these factors, individuals can experience a greater sense of balance and well-being.
- Increased self-awareness:Mental health examinations can provide individuals with valuable insights into their own mental health, promoting self-awareness and understanding. This increased awareness can empower individuals to make informed decisions about their mental health and seek appropriate support when needed.
- Improved relationships:Mental health concerns can negatively impact relationships with family, friends, and colleagues. Mental health examinations can help individuals develop healthier coping mechanisms and communication skills, improving their relationships and fostering a stronger sense of connection.
- Enhanced productivity and performance:Mental health issues can significantly affect productivity and performance at work, school, and in other areas of life. By addressing mental health concerns early on, individuals can maintain their productivity and achieve their goals more effectively.
- Greater life satisfaction:Mental health is an integral part of overall well-being. By prioritizing mental health, individuals can experience greater life satisfaction, feeling more content, fulfilled, and connected to their purpose.
Components of a Mental Health Examination Template
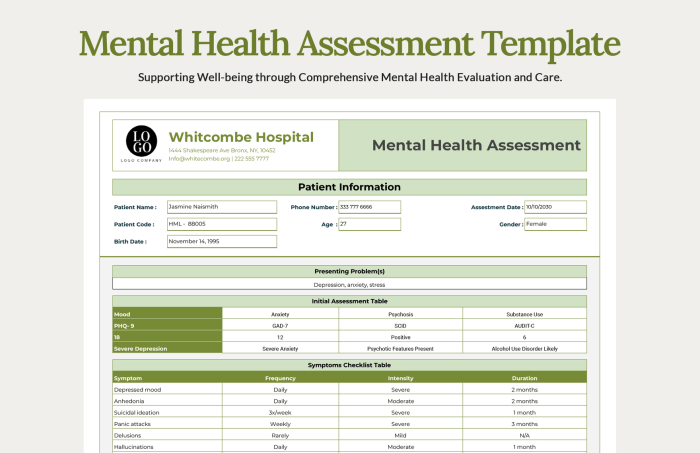
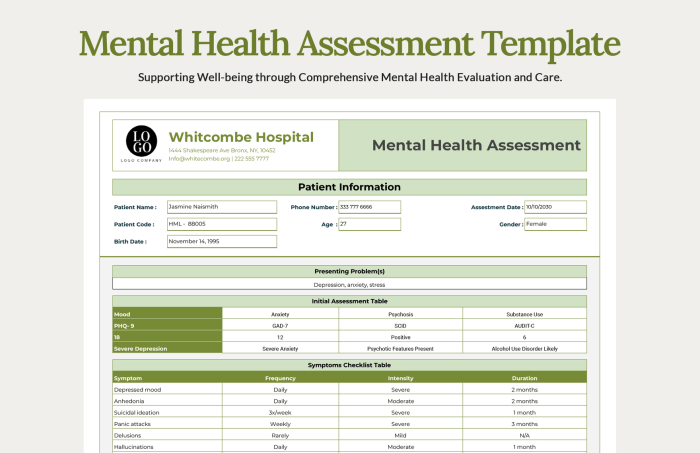
A comprehensive mental health examination template is a structured tool used by mental health professionals to gather essential information about a patient’s mental well-being. This template ensures a thorough assessment, enabling clinicians to understand the patient’s history, current symptoms, and potential contributing factors, leading to effective diagnosis and treatment planning.
Demographics
This section collects basic information about the patient, such as their name, age, gender, race, ethnicity, marital status, occupation, and contact information. This information helps establish the patient’s background and context.
Presenting Concerns
This section focuses on the primary reasons for the patient’s visit. It details the specific symptoms, concerns, or problems the patient is experiencing. This includes the onset, duration, severity, and impact of the symptoms on the patient’s daily life.
Mental Health History
This section delves into the patient’s past experiences with mental health conditions. It includes information on previous diagnoses, treatments received, medications taken, and their effectiveness. It also explores the patient’s history of mental health services utilization, such as therapy, hospitalization, or support groups.
Physical Health History
This section gathers information about the patient’s physical health, including any chronic conditions, surgeries, medications, and allergies. This is crucial as physical health can significantly impact mental health, and vice versa. For example, chronic pain can lead to depression, while anxiety can exacerbate physical health problems.
Family History
This section explores the patient’s family history of mental and physical health conditions. This information is valuable as it helps identify potential genetic predispositions and risk factors for mental health issues. For example, a family history of depression or anxiety can increase the likelihood of developing these conditions.
Social History
This section examines the patient’s social environment, including their relationships, support system, and social activities. It explores aspects like family dynamics, friendships, work or school life, and involvement in community activities. This information helps understand the patient’s social support network and how it might influence their mental health.
Substance Use History
This section assesses the patient’s history of substance use, including alcohol, drugs, and nicotine. It inquires about patterns of use, frequency, and any associated problems or dependence. This information is vital as substance use can significantly impact mental health and vice versa.
Legal History
This section gathers information about the patient’s legal history, including any arrests, convictions, or involvement with the legal system. This information can provide insights into potential risk factors for mental health issues and inform treatment planning.
Educational History
This section explores the patient’s educational background, including their level of education, academic performance, and any learning difficulties. This information can help understand the patient’s cognitive abilities and potential impact on their mental health.
Occupational History
This section gathers information about the patient’s work history, including their current and past jobs, work satisfaction, and any work-related stressors. This information can provide insights into the patient’s coping mechanisms and potential impact of work on their mental health.
A comprehensive mental health examination template should include a range of assessments to gain a thorough understanding of an individual’s well-being. One crucial aspect to consider is the individual’s awareness of their mental health, which can be assessed through tools like the mental health AWA.
This type of assessment helps to identify potential areas of concern and can be incorporated into the overall mental health examination template for a more holistic approach.
Cultural and Spiritual History
This section explores the patient’s cultural and spiritual background, including their beliefs, values, and practices. This information is crucial for understanding the patient’s perspective on mental health and how their culture might influence their experiences and treatment preferences.
Current Medications
This section lists all the medications the patient is currently taking, including dosage, frequency, and purpose. This information is essential for understanding potential interactions with mental health medications and ensuring patient safety.
Mental Status Examination
This section is a structured assessment of the patient’s current mental state. It includes observations of their appearance, behavior, speech, mood, affect, thought processes, cognition, and insight. This comprehensive evaluation provides valuable information about the patient’s mental functioning and potential diagnoses.
Risk Assessment
This section assesses the patient’s risk for suicide, self-harm, or harm to others. It includes questions about suicidal thoughts, plans, or attempts, as well as any history of violence or aggression. This information is crucial for ensuring patient safety and implementing appropriate interventions.
Treatment Plan
This section Artikels the proposed treatment plan based on the patient’s assessment. It includes recommendations for therapy, medication, and other interventions, such as support groups or lifestyle changes. The treatment plan should be individualized to meet the patient’s specific needs and goals.
Documentation
This section includes all the documentation related to the patient’s assessment, including notes, test results, and treatment plans. It ensures a comprehensive record of the patient’s care and facilitates communication between healthcare providers.
Assessment Tools and Techniques
Mental health examinations rely on a variety of tools and techniques to gather information about a person’s mental state and well-being. These assessments help mental health professionals understand the nature and severity of mental health issues, develop effective treatment plans, and monitor progress over time.
Standardized Questionnaires
Standardized questionnaires are structured assessments that consist of a set of questions with predetermined response options. They provide a systematic and objective way to gather information about a person’s thoughts, feelings, and behaviors.
- Advantages:Standardized questionnaires offer several advantages, including their efficiency, objectivity, and ease of administration. They can be administered quickly and scored reliably, allowing for comparisons across individuals. They also reduce the risk of bias introduced by subjective interpretation.
- Limitations:While standardized questionnaires are valuable tools, they also have limitations. They may not capture the nuances of individual experiences, and individuals may provide socially desirable responses. Additionally, they may not be suitable for all individuals, such as those with limited literacy skills or cognitive impairments.
Examples of commonly used standardized questionnaires include:
- Beck Depression Inventory (BDI):Measures the severity of depressive symptoms.
- Generalized Anxiety Disorder-7 (GAD-7):Screens for generalized anxiety disorder.
- Patient Health Questionnaire (PHQ-9):Assesses the severity of depressive symptoms.
Clinical Interviews
Clinical interviews are structured or semi-structured conversations between a mental health professional and the individual being assessed. These interviews provide a more in-depth understanding of the person’s history, symptoms, and experiences.
- Advantages:Clinical interviews allow for a comprehensive assessment, enabling mental health professionals to explore the individual’s unique circumstances and perspectives. They provide opportunities for clarification, follow-up questions, and observation of nonverbal cues.
- Limitations:Clinical interviews can be time-consuming and may be influenced by the interviewer’s biases. They also rely on the individual’s willingness and ability to provide accurate and complete information.
Examples of commonly used clinical interview techniques include:
- Mental Status Examination (MSE):A structured assessment of the individual’s appearance, behavior, speech, thought processes, mood, and affect.
- Structured Clinical Interview for DSM-5 (SCID):A standardized interview used to diagnose mental disorders based on the Diagnostic and Statistical Manual of Mental Disorders (DSM-5).
Psychological Tests
Psychological tests are standardized measures designed to assess various aspects of an individual’s cognitive, emotional, and behavioral functioning. They provide objective data that can be used to understand underlying psychological processes and identify potential areas of concern.
- Advantages:Psychological tests offer a standardized and objective way to measure specific psychological constructs. They can be used to identify strengths and weaknesses, assess cognitive abilities, and measure personality traits.
- Limitations:Psychological tests should be interpreted cautiously, as they may not always accurately reflect an individual’s true abilities or personality. It is important to consider the test’s reliability, validity, and cultural appropriateness.
Examples of commonly used psychological tests include:
- Wechsler Adult Intelligence Scale (WAIS):Measures general cognitive ability in adults.
- Minnesota Multiphasic Personality Inventory (MMPI):Assesses personality traits and psychopathology.
- Thematic Apperception Test (TAT):A projective test that explores unconscious motives and conflicts.
Interpretation and Diagnosis
The interpretation of assessment data and formulation of a diagnosis are crucial steps in the mental health examination process. This involves analyzing the collected information, identifying patterns, and determining whether the observed symptoms meet the criteria for a specific mental health condition.
Criteria for Identifying Mental Health Conditions
The Diagnostic and Statistical Manual of Mental Disorders (DSM-5) provides a standardized framework for diagnosing mental health conditions. It Artikels specific criteria that must be met for a diagnosis to be made. These criteria include:* Duration:The symptoms must persist for a certain period of time.
A comprehensive mental health examination template can be a valuable tool for healthcare professionals. It helps ensure a thorough assessment, covering aspects like mood, anxiety, and sleep patterns. For individuals seeking support in maintaining a healthy lifestyle, am fam fitness offers a holistic approach, incorporating physical activity and mental well-being.
By understanding the interconnectedness of these factors, a mental health examination template can play a crucial role in promoting overall well-being.
Severity
The symptoms must be significant enough to cause distress or impairment in daily functioning.
Exclusion of other conditions
The symptoms must not be better explained by another medical or mental health condition.
Clinical significance
The symptoms must be considered clinically significant, meaning they are not simply normal variations in behavior or mood.
Cultural and Contextual Factors in Diagnosis
It is essential to consider cultural and contextual factors when interpreting assessment data and formulating a diagnosis. Cultural norms and beliefs can influence how individuals express their symptoms, and what is considered “normal” behavior can vary across cultures. For example, some cultures may view certain symptoms, such as anxiety or depression, as a sign of weakness or shame, which can lead to underreporting or delayed help-seeking.
It is important to approach diagnosis with cultural sensitivity and avoid imposing Western-centric views on individuals from different cultural backgrounds.
Additionally, contextual factors, such as socioeconomic status, education level, and life experiences, can also influence mental health. For example, individuals living in poverty or experiencing discrimination may be at increased risk for developing certain mental health conditions.
Assessment Tools and Techniques
A variety of assessment tools and techniques can be used to gather information about an individual’s mental health. These include:* Interviews:Structured or semi-structured interviews allow clinicians to gather detailed information about an individual’s symptoms, history, and current functioning.
Questionnaires
Self-report questionnaires allow individuals to provide information about their own experiences and symptoms.
Psychological tests
Standardized tests can assess cognitive abilities, personality traits, and emotional functioning.
Observation
Clinicians can observe an individual’s behavior and interactions to gain insights into their mental state.The specific assessment tools and techniques used will depend on the individual’s presenting concerns and the purpose of the evaluation.
Formulating a Diagnosis
After gathering information through assessment, clinicians use their clinical judgment and the criteria Artikeld in the DSM-5 to formulate a diagnosis. This process involves:* Synthesizing the information:Analyzing the collected data to identify patterns and trends.
A comprehensive mental health examination template can help assess a client’s overall well-being, but it’s important to consider their financial situation as well. For instance, if a client is looking to improve their physical health, they might be interested in exploring options like a Crunch Fitness membership, which offers various plans and prices here.
Ultimately, a successful mental health plan should consider both the client’s mental and physical needs, and affordability is a crucial factor in achieving both.
Considering differential diagnoses
Ruling out other possible conditions that may explain the symptoms.
Determining the severity of the condition
Assessing the impact of the symptoms on the individual’s daily functioning.
Developing a treatment plan
Based on the diagnosis, clinicians develop a treatment plan that addresses the individual’s specific needs.
It is important to note that a diagnosis is not a label but rather a tool to help understand and treat an individual’s mental health condition.
Treatment Planning and Recommendations
The treatment plan is the roadmap for addressing a patient’s mental health concerns. It Artikels the specific strategies and interventions aimed at alleviating symptoms, improving overall well-being, and promoting recovery.
Components of a Treatment Plan
The treatment plan is a collaborative effort between the mental health professional and the patient. It is tailored to the individual’s needs, preferences, and circumstances. The plan typically includes:
Therapy Recommendations
- Psychotherapy:This involves talking therapy with a qualified mental health professional to explore thoughts, feelings, and behaviors. Different types of psychotherapy, such as cognitive-behavioral therapy (CBT), psychodynamic therapy, and interpersonal therapy (IPT), can be tailored to specific conditions.
- Group Therapy:Group therapy provides a supportive environment for individuals with similar concerns to share experiences, learn coping skills, and build social connections.
- Family Therapy:Family therapy addresses issues within the family unit, improving communication and dynamics to support the patient’s recovery.
Medication Management
- Psychotropic Medications:Prescribed by psychiatrists or other qualified healthcare providers, these medications can help regulate neurotransmitters and alleviate symptoms.
- Medication Monitoring:Regular checkups are essential to monitor the effectiveness of medications, adjust dosages, and manage potential side effects.
Lifestyle Interventions
- Healthy Diet:A balanced diet can positively impact mood and energy levels.
- Regular Exercise:Physical activity releases endorphins, reducing stress and improving mood.
- Sufficient Sleep:Adequate sleep is crucial for mental well-being and cognitive function.
- Stress Management Techniques:Techniques such as yoga, meditation, and deep breathing exercises can help manage stress and anxiety.
Individualized Treatment Plans
“Every individual is unique, and their treatment plan should reflect their specific needs and preferences.”
Treatment plans are not one-size-fits-all. The mental health professional will consider the patient’s:
- Diagnosis:The specific mental health condition diagnosed.
- Symptoms:The severity and nature of the patient’s symptoms.
- Personal History:Past experiences, coping mechanisms, and support systems.
- Values and Preferences:The patient’s beliefs, goals, and desired outcomes.
- Cultural Background:Cultural beliefs and practices that may influence treatment preferences.
Treatment Strategies for Mental Health Conditions, Mental health examination template
Anxiety Disorders
- Cognitive-Behavioral Therapy (CBT):Helps identify and challenge negative thought patterns and develop coping mechanisms.
- Exposure Therapy:Gradually exposes the individual to feared situations to reduce anxiety.
- Medications:Anti-anxiety medications, such as benzodiazepines and selective serotonin reuptake inhibitors (SSRIs), can provide short-term relief.
Depression
- Psychotherapy:CBT, interpersonal therapy (IPT), and psychodynamic therapy can address negative thoughts, improve interpersonal relationships, and enhance coping skills.
- Medications:Antidepressants, such as SSRIs, serotonin-norepinephrine reuptake inhibitors (SNRIs), and tricyclic antidepressants (TCAs), can help regulate mood.
- Electroconvulsive Therapy (ECT):A more intensive treatment option for severe depression that involves inducing a brief seizure.
Bipolar Disorder
- Mood Stabilizers:Medications such as lithium, valproic acid, and lamotrigine help regulate mood swings.
- Antipsychotics:May be used to manage psychotic symptoms during manic episodes.
- Psychotherapy:CBT, family therapy, and psychoeducation can help patients understand their condition, manage symptoms, and improve coping skills.
Schizophrenia
- Antipsychotic Medications:These medications help reduce hallucinations, delusions, and disorganized thinking.
- Psychotherapy:CBT, family therapy, and social skills training can help improve social functioning and reduce symptoms.
- Psychosocial Rehabilitation:Provides support and training to help individuals with schizophrenia live fulfilling lives.
Documentation and Record Keeping
Thorough documentation is crucial in mental health examinations, forming the foundation for effective treatment, communication, and legal protection. It provides a comprehensive record of the patient’s journey, enabling healthcare professionals to understand their history, progress, and needs.
Importance of Documentation
Documentation plays a vital role in ensuring continuity of care, facilitating communication between healthcare providers, and safeguarding the patient’s rights. It allows for accurate record-keeping, enabling practitioners to monitor the patient’s progress, identify potential issues, and adjust treatment plans accordingly.
Essential Information in Patient Records
Patient records should encompass a wide range of information, including:
- Assessment Findings:This includes detailed observations of the patient’s mental and emotional state, including symptoms, behaviors, and cognitive functioning.
- Diagnosis:The diagnosis, based on the assessment findings and established criteria, provides a framework for understanding the patient’s condition and guiding treatment decisions.
- Treatment Plan:This Artikels the specific interventions, therapies, and medications chosen to address the patient’s needs. It should be tailored to the individual and regularly reviewed and updated as progress is made.
- Progress Notes:These notes document the patient’s progress, including changes in symptoms, response to treatment, and any significant events or interactions.
Legal and Ethical Considerations
Documentation in mental health care is subject to specific legal and ethical considerations. It is essential to ensure that records are:
- Accurate and Complete:Entries should be factual, objective, and reflect the actual observations and assessments.
- Confidentiality:Patient information must be kept confidential and protected from unauthorized access. This includes adhering to HIPAA regulations and maintaining secure storage practices.
- Informed Consent:Patients must be informed about the purpose of documentation, the types of information collected, and their right to access their records.
Ethical Considerations in Mental Health Examinations
Mental health examinations are crucial for diagnosing and treating mental health conditions. However, they must be conducted ethically, respecting the rights and dignity of individuals seeking care. Ethical principles serve as a framework to guide mental health professionals in their assessments, ensuring that patients are treated with respect and their well-being is prioritized.
Confidentiality and Privacy
Confidentiality is paramount in mental health assessments. It refers to the obligation of mental health professionals to keep information shared by patients private and not disclose it to others without their consent. This includes any personal information, medical history, diagnoses, and treatment plans.
Patients should feel safe and comfortable sharing sensitive information with their therapist, knowing that it will be protected.
- Exceptions to Confidentiality:While confidentiality is a cornerstone of ethical practice, there are exceptions. For example, if a patient poses a danger to themselves or others, the therapist may be obligated to break confidentiality to ensure safety. This is often referred to as the “duty to warn” principle.
In cases of child abuse or neglect, the therapist may also be required to report it to the authorities.
- HIPAA:The Health Insurance Portability and Accountability Act (HIPAA) is a federal law that sets standards for protecting sensitive patient health information. Mental health professionals are required to comply with HIPAA regulations, which include provisions for obtaining informed consent for the use and disclosure of patient information.
Informed Consent
Informed consent is a fundamental ethical principle in healthcare. It ensures that patients understand the nature of the assessment, the potential risks and benefits, and have the opportunity to make an informed decision about whether to proceed.
- Process:Informed consent is a process that involves explaining the assessment procedure, the purpose, and the potential outcomes. It also includes discussing any risks or potential discomfort associated with the assessment, as well as the patient’s rights to refuse or withdraw from the assessment at any time.
- Documentation:Informed consent should be documented in the patient’s medical record. This documentation should include the date, the nature of the information provided, and the patient’s signature indicating their understanding and agreement.
Patient Autonomy
Patient autonomy refers to the right of individuals to make their own decisions about their healthcare. This includes the right to choose their treatment, to refuse treatment, and to participate in decisions about their care.
- Respect for Choices:Mental health professionals must respect the patient’s choices, even if they differ from the therapist’s recommendations. The therapist should provide information and support to help the patient make informed decisions, but ultimately, the decision-making power rests with the patient.
- Shared Decision-Making:Shared decision-making is a collaborative process where the therapist and the patient work together to make decisions about the patient’s care. This involves open communication, active listening, and considering the patient’s values and preferences.
Cultural Sensitivity and Respect for Diversity
Mental health care must be culturally sensitive and respectful of diversity. This means recognizing and acknowledging the unique cultural backgrounds, beliefs, and experiences of individuals seeking care.
- Cultural Influences:Mental health presentations can vary across cultures. What may be considered a mental illness in one culture may not be in another. Therapists should be aware of these cultural differences and avoid imposing their own cultural biases on patients.
- Cultural Competence:Cultural competence involves developing an understanding of different cultures and their impact on mental health. This includes learning about cultural beliefs about mental illness, cultural norms for communication and expression, and culturally appropriate treatment approaches.
Ethical Dilemmas
Ethical dilemmas can arise in mental health examinations. These are situations where there are competing ethical principles, and it is difficult to determine the best course of action.
- Confidentiality vs. Duty to Warn:A therapist may be faced with a situation where a patient reveals a threat to harm themselves or others. The therapist has a duty to protect the patient and others, but this may require breaking confidentiality.
- Dual Relationships:Dual relationships occur when a therapist has a personal or professional relationship with a patient outside of the therapeutic relationship. These relationships can create conflicts of interest and may compromise the therapist’s objectivity.
Legal and Regulatory Frameworks: Mental Health Examination Template
Mental health examinations are conducted within a complex legal and regulatory framework that aims to protect the rights of individuals while ensuring the ethical and responsible practice of mental health professionals. This framework encompasses a variety of laws, regulations, and professional guidelines that govern various aspects of the examination process.
Privacy Laws
Privacy laws are crucial in safeguarding the confidentiality and security of patient information. These laws dictate how personal health information, including mental health records, can be collected, used, disclosed, and stored. The Health Insurance Portability and Accountability Act (HIPAA) in the United States, for instance, establishes national standards for protecting sensitive patient health information.
Similarly, the General Data Protection Regulation (GDPR) in the European Union provides comprehensive data protection for individuals within the EU. These laws impose strict requirements on mental health professionals regarding the handling and disclosure of patient information, emphasizing the importance of obtaining informed consent before accessing or sharing any sensitive data.
Informed Consent
Informed consent is a fundamental principle in mental health practice, ensuring that individuals understand the nature and implications of the examination process before participating. This involves providing clear and concise information about the purpose, procedures, potential risks and benefits, and alternative options associated with the examination.
Individuals must be given the opportunity to ask questions and receive answers in a way they can understand. The informed consent process should be documented, with a signed consent form serving as evidence of the patient’s voluntary participation.
Reporting Obligations
Mental health professionals may have legal obligations to report certain information, such as suspected child abuse or neglect, elder abuse, or threats of harm to oneself or others. These reporting obligations are designed to protect vulnerable individuals and ensure their safety.
Failure to comply with reporting requirements can result in legal penalties. The specific reporting requirements vary depending on the jurisdiction and the nature of the information being reported.
Professional Organizations and Licensing Boards
Professional organizations and licensing boards play a vital role in setting ethical and professional standards for mental health practice. These organizations establish codes of ethics, guidelines for practice, and continuing education requirements to ensure that mental health professionals maintain their competence and adhere to ethical principles.
Licensing boards are responsible for granting and regulating licenses to mental health professionals, ensuring that they meet specific qualifications and standards. Violation of ethical and professional standards can lead to disciplinary actions, including license suspension or revocation.
Legal Consequences of Violations
Violating ethical and legal guidelines in mental health examinations can have serious legal consequences. These consequences can range from professional sanctions, such as reprimands or license suspension, to civil lawsuits for negligence or malpractice. In some cases, criminal charges may be filed, particularly in situations involving breaches of confidentiality, fraud, or abuse.
It is therefore essential for mental health professionals to stay informed about relevant laws and regulations and to adhere to ethical principles in their practice.
Examples of Mental Health Examination Templates
Mental health examination templates are crucial tools for mental health professionals, providing a standardized framework for conducting comprehensive assessments. These templates guide practitioners in gathering essential information, ensuring consistency and accuracy in diagnosis and treatment planning.
Types of Mental Health Examination Templates
Various templates cater to specific needs and populations. Here’s a table highlighting some common examples:
| Template Type | Target Population | Key Features | Download Link |
|---|---|---|---|
| Adult Mental Health Assessment | Adults experiencing mental health concerns | Comprehensive assessment covering mood, anxiety, psychosis, and substance use | [Link to a reliable source for download] |
| Child and Adolescent Mental Health Assessment | Children and adolescents with mental health issues | Focuses on developmental milestones, behavioral problems, and family history | [Link to a reliable source for download] |
| Geriatric Mental Health Assessment | Older adults with mental health concerns | Includes cognitive function, memory, and physical health considerations | [Link to a reliable source for download] |
| Forensic Mental Health Assessment | Individuals involved in legal proceedings | Evaluates competency to stand trial, criminal responsibility, and risk assessment | [Link to a reliable source for download] |
Future Directions in Mental Health Examinations
The field of mental health assessment is constantly evolving, driven by technological advancements and a growing understanding of the complexities of mental well-being. This evolution is paving the way for more comprehensive, personalized, and effective approaches to mental health care.
Technology and Digital Tools
The integration of technology and digital tools is transforming the landscape of mental health examinations. These tools offer several advantages, including:
- Increased accessibility:Online platforms and mobile applications provide convenient access to mental health assessments, reducing geographical barriers and stigma associated with seeking help. This is especially important for individuals in remote areas or with limited access to traditional healthcare services.
- Improved efficiency:Digital tools streamline the assessment process, automating tasks such as data collection, scoring, and report generation, freeing up clinicians’ time for more personalized interactions with patients.
- Enhanced objectivity:Technology can help reduce subjective biases in assessments by providing standardized and objective measurements. For example, wearable sensors can track physiological data like sleep patterns and heart rate variability, offering valuable insights into mental health.
- Personalized interventions:Digital tools allow for the development of personalized interventions tailored to individual needs and preferences. For instance, mobile apps can provide tailored exercises, mindfulness practices, and cognitive behavioral therapy (CBT) modules based on an individual’s assessment results.
Artificial Intelligence and Machine Learning
Artificial intelligence (AI) and machine learning (ML) are emerging as powerful tools in mental health assessment. These technologies can analyze vast amounts of data to identify patterns and predict outcomes, leading to more accurate and early diagnoses.
- Automated screening and diagnosis:AI-powered algorithms can analyze speech patterns, facial expressions, and other behavioral cues to identify individuals at risk of mental health conditions. This can facilitate early intervention and prevent the escalation of symptoms.
- Personalized treatment recommendations:AI can analyze patient data and research literature to recommend personalized treatment plans based on individual characteristics, symptoms, and response to previous interventions.
- Predictive analytics:AI can predict the likelihood of relapse or future mental health challenges, enabling proactive interventions and support for individuals at risk.
Future Direction of Mental Health Assessment
The future of mental health assessment is likely to be characterized by a greater emphasis on:
- Holistic assessment:Moving beyond traditional symptom-based assessments to consider a broader range of factors, including social determinants of health, cultural background, and personal experiences.
- Prevention and early intervention:Focusing on identifying individuals at risk of mental health challenges early on and providing timely interventions to prevent the development of more severe conditions.
- Person-centered care:Tailoring assessments and interventions to meet the unique needs and preferences of each individual.
- Integration of technology:Leveraging technology to enhance the accessibility, efficiency, and effectiveness of mental health assessments and interventions.
Ultimate Conclusion
Mental health examination templates are indispensable tools for mental health professionals, offering a systematic approach to comprehensive assessments. By utilizing these templates, clinicians can ensure thorough evaluations, accurate diagnoses, and individualized treatment plans. The adoption of such templates contributes to the advancement of mental health care, promoting greater understanding, improved outcomes, and a more holistic approach to patient well-being.
Clarifying Questions
What are the benefits of using a mental health examination template?
Using a mental health examination template ensures consistency in assessments, facilitates accurate diagnoses, and promotes effective treatment planning. It also helps clinicians gather all relevant information and improve patient care.
How often should mental health examinations be conducted?
The frequency of mental health examinations depends on the individual’s needs and the severity of their condition. Regular assessments are crucial for individuals with ongoing mental health concerns, while those with less severe issues may require less frequent evaluations.
Can I use a mental health examination template for self-assessment?
While mental health examination templates can be helpful for self-reflection, they should not be used as a substitute for professional evaluation. It’s essential to consult with a qualified mental health professional for a comprehensive assessment.