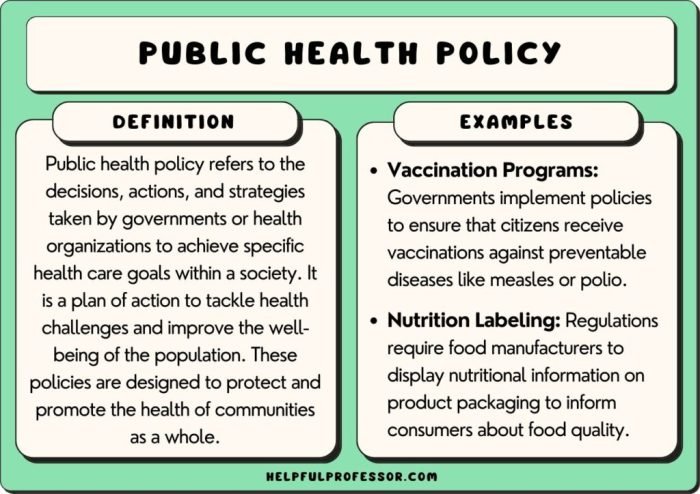
Policies and health are intertwined, shaping the very fabric of our lives. From government regulations to healthcare access, policies have a profound impact on our health outcomes. This exploration delves into the intricate relationship between policy and health, examining how policies can both positively and negatively influence our well-being.
We’ll investigate the frameworks that guide policy development, dissect current health policy issues and debates, and explore the crucial role of evaluation and advocacy in shaping a healthier future.
Understanding the complex interplay between policies and health is essential for building a society that prioritizes the well-being of its citizens. This journey will illuminate the multifaceted nature of this relationship, showcasing the power of policy to both hinder and advance public health.
Impact of Policies on Health

Government policies play a crucial role in shaping public health outcomes. They can either promote health and well-being or contribute to health disparities and inequalities.
Policies that promote health and wellness are crucial for creating a thriving community. One great example is the m health fairview sports center , which provides access to various fitness programs and resources, ultimately contributing to the overall well-being of its members.
By supporting such initiatives, we can foster a culture that prioritizes health and encourages individuals to make healthy choices.
Positive Impacts of Policies on Health
Policies can significantly impact health outcomes positively. Here are some examples:
- Smoking Bans: Implementing comprehensive smoke-free policies in public places and workplaces has been proven to reduce tobacco use and its associated health risks. These policies protect non-smokers from secondhand smoke exposure and encourage smokers to quit.
- Vaccination Mandates: Mandatory vaccination programs have played a vital role in eradicating or controlling infectious diseases, such as polio, measles, and rubella. These mandates protect individuals and communities by ensuring high vaccination coverage, preventing outbreaks, and reducing the spread of diseases.
- Healthcare Access Programs: Policies aimed at expanding access to affordable healthcare, such as Medicaid and the Affordable Care Act, have increased insurance coverage and improved access to preventive care, screenings, and treatment for millions of Americans. These programs have reduced health disparities and improved overall health outcomes.
Negative Impacts of Policies on Health
Policies can also have unintended negative consequences for health.
Policies aimed at improving public health often focus on preventative measures, encouraging healthy lifestyles. This can include promoting access to resources like fitness centers or, as seen in the beauty house concept, emphasizing holistic well-being. Ultimately, policies that promote both physical and mental health contribute to a stronger and more resilient society.
- Budget Cuts to Public Health Programs: Reducing funding for public health programs can lead to weakened surveillance systems, reduced access to preventive services, and a decline in the quality of public health infrastructure. This can result in increased disease outbreaks, health disparities, and higher healthcare costs.
- Environmental Regulations: Weakening environmental regulations can lead to increased air and water pollution, which can contribute to respiratory illnesses, cardiovascular diseases, and other health problems. Environmental degradation can also negatively impact mental health and well-being.
- Access to Healthy Food: Policies that restrict access to healthy food, such as limiting food assistance programs or promoting unhealthy food options in schools, can contribute to diet-related diseases, such as obesity, diabetes, and heart disease.
Case Study: Impact of Smoke-Free Policies on Heart Health
A study conducted in the United Kingdom found that the implementation of smoke-free policies in public places was associated with a significant reduction in hospital admissions for heart attacks. The study, published in the journal “The Lancet,” analyzed data from over 10 years before and after the introduction of smoke-free legislation in 2007.
The researchers found that the number of heart attack hospitalizations decreased by 17% in the year following the implementation of the smoke-free policy. This reduction was attributed to the decreased exposure to secondhand smoke, which is a known risk factor for heart disease.
Health Policy Frameworks

Health policy frameworks provide a structured approach to guide the development and implementation of health policies. They offer a set of principles, tools, and strategies to address health challenges effectively. These frameworks serve as blueprints for policymakers, highlighting key areas of focus and guiding the allocation of resources.
World Health Organization’s Health Systems Framework
The World Health Organization’s (WHO) Health Systems Framework provides a comprehensive model for understanding and strengthening health systems. This framework emphasizes six building blocks:
- Leadership and Governance: This element focuses on the effective leadership and management of health systems, including policy development, resource allocation, and accountability.
- Health Financing: This building block explores the sources of funding for health services, including government budgets, insurance schemes, and out-of-pocket payments. It also addresses the efficiency and equity of financing mechanisms.
- Health Workforce: This aspect examines the availability, distribution, and competence of healthcare professionals. It emphasizes the importance of training, education, and retention of qualified personnel.
- Medical Products, Vaccines, and Technologies: This building block addresses the availability, quality, and safety of essential medical products, vaccines, and technologies. It includes considerations for procurement, supply chain management, and rational use.
- Information Systems: This element focuses on the collection, analysis, and use of health data for decision-making, monitoring, and evaluation. Effective information systems are crucial for tracking health outcomes, identifying trends, and improving efficiency.
- Service Delivery: This building block examines the organization and delivery of healthcare services, including primary care, secondary care, and tertiary care. It addresses the accessibility, quality, and responsiveness of services to meet the needs of the population.
The WHO’s Health Systems Framework provides a valuable tool for analyzing health system performance, identifying strengths and weaknesses, and prioritizing areas for improvement. This framework has been widely adopted by countries around the world, serving as a basis for national health policy development and implementation.
Health in All Policies
The Health in All Policies (HiAP) approach recognizes the interconnectedness of health with other sectors, such as education, transportation, and environment. It emphasizes the importance of integrating health considerations into policies across all government departments.
- Key Principles of HiAP:
- Multi-sectoral collaboration: HiAP promotes collaboration between different government departments and stakeholders to address health determinants in a holistic manner.
- Health equity: This approach aims to reduce health disparities and ensure equitable access to health services and opportunities.
- Prevention and early intervention: HiAP emphasizes prevention and early intervention strategies to address health challenges before they become more serious and costly.
- Sustainability: This approach aims to promote policies that are sustainable and support long-term health outcomes.
- Target Areas for HiAP:
- Urban planning: Policies related to urban planning can influence physical activity, air quality, and access to healthy food.
- Transportation: Policies promoting active transportation, such as walking and cycling, can improve physical health and reduce traffic-related injuries.
- Education: Education policies can influence health literacy, healthy behaviors, and access to healthcare services.
- Environment: Policies aimed at protecting the environment can reduce exposure to pollution, improve air quality, and promote healthy lifestyles.
HiAP provides a valuable framework for addressing the social determinants of health and promoting a holistic approach to health policy development. It encourages a collaborative and multi-sectoral approach to creating healthier environments and societies.
Comparison of Health Policy Frameworks
| Framework | Key Principles | Target Areas | Examples of Application |
|---|---|---|---|
| WHO’s Health Systems Framework | Leadership and governance, health financing, health workforce, medical products, information systems, service delivery | Strengthening health systems, improving health outcomes, promoting equity | National health plans, health system reforms, quality improvement initiatives |
| Health in All Policies | Multi-sectoral collaboration, health equity, prevention and early intervention, sustainability | Addressing social determinants of health, promoting healthy environments, reducing health disparities | Urban planning policies, transportation policies, education policies, environmental policies |
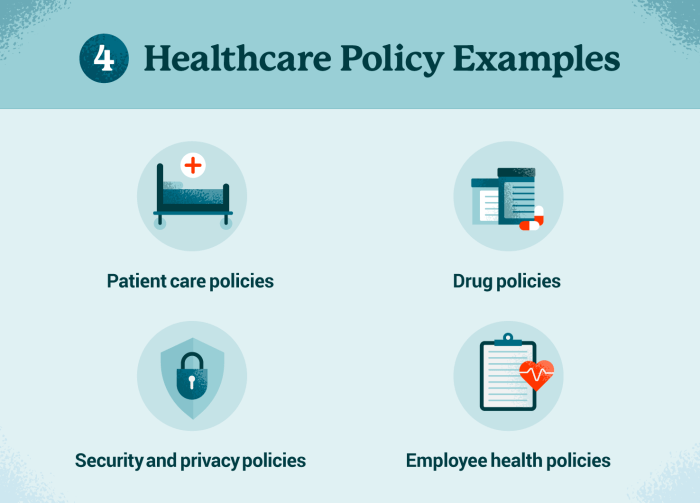
Health Policy Issues and Debates
Health policy issues are complex and often contentious, reflecting the diverse values and priorities of stakeholders. These issues are constantly evolving, influenced by factors such as technological advancements, changing demographics, and economic conditions. Understanding the various perspectives and arguments surrounding these issues is crucial for informed policymaking and advocacy.
Access to Healthcare
Access to healthcare is a fundamental right, but disparities persist in many countries. Factors such as socioeconomic status, geographic location, and insurance coverage can significantly impact access to quality healthcare services. This explores the challenges and debates surrounding access to healthcare.
- Cost of Healthcare: The rising cost of healthcare is a major barrier to access, particularly for low-income individuals and families. Policymakers face the challenge of balancing affordability with the need to ensure quality care. Some argue for universal healthcare systems, while others advocate for market-based solutions.
- Insurance Coverage: The availability and affordability of health insurance are critical determinants of access to healthcare. Different models of insurance coverage exist, ranging from employer-sponsored plans to government-funded programs. Policy debates often center around the role of the government in providing health insurance and the balance between individual responsibility and social solidarity.
- Geographic Accessibility: Access to healthcare can be limited by geographic factors, particularly in rural or underserved areas. This issue involves considerations of healthcare infrastructure, provider availability, and transportation options. Policies aimed at addressing this challenge often involve incentives for providers to practice in underserved areas or the use of telehealth technologies.
Cost Containment
Healthcare costs have been rising steadily in many countries, posing a significant burden on individuals, employers, and governments. This examines the various strategies and debates surrounding cost containment in healthcare.
Government policies can have a significant impact on health outcomes, including encouraging healthy dietary choices. One area where this is particularly important is seafood consumption, as fish is a rich source of essential nutrients. If you’re looking for delicious and healthy ways to incorporate fish into your diet, check out these health fish recipes.
By making informed choices about our food, we can contribute to both our personal well-being and the overall health of our communities.
- Price Transparency: Advocates for price transparency argue that increased disclosure of healthcare pricing information can empower consumers to make informed choices and drive competition among providers. However, concerns exist regarding the complexity of pricing structures and the potential for price gouging.
- Value-Based Care: This approach focuses on rewarding providers based on the quality and efficiency of care rather than simply the volume of services provided. The goal is to improve outcomes and reduce unnecessary costs. However, challenges remain in developing and implementing effective value-based care models.
- Drug Pricing: The high cost of prescription drugs is a major contributor to overall healthcare spending. Policy debates on drug pricing revolve around issues such as patent protection, government negotiation power, and the role of generics.
Mental Health
Mental health conditions are prevalent, but access to mental healthcare services often lags behind physical healthcare. This examines the challenges and debates surrounding mental health policy.
- Stigma and Discrimination: Mental health stigma remains a significant barrier to seeking help. Policies aimed at reducing stigma include public education campaigns, increased awareness, and the promotion of mental health literacy.
- Integration of Mental and Physical Healthcare: Integrating mental health services into primary care settings is seen as a promising approach to improve access and reduce fragmentation of care. However, challenges exist in training primary care providers and ensuring adequate resources for mental health services.
- Access to Specialized Services: Individuals with severe mental illness may require specialized services, such as inpatient care, medication management, and psychosocial rehabilitation. Policy debates often focus on the availability and accessibility of these services, particularly in underserved communities.
Chronic Disease Management
Chronic diseases, such as diabetes, heart disease, and cancer, are a growing public health concern. This explores the challenges and debates surrounding chronic disease management policies.
- Prevention and Early Detection: Preventing chronic diseases and detecting them early are crucial for improving outcomes and reducing healthcare costs. Policies often focus on public health interventions, such as promoting healthy lifestyles, early screening programs, and access to preventive services.
- Patient Empowerment and Self-Management: Empowering patients to actively manage their chronic conditions is essential for improving health outcomes. Policies may involve patient education, self-management support programs, and access to technology that facilitates self-monitoring and communication with healthcare providers.
- Coordination of Care: Effective chronic disease management requires coordinated care across different healthcare settings. Policies aimed at improving coordination may involve the use of electronic health records, care coordination teams, and patient-centered care models.
Health Policy Evaluation and Monitoring
Evaluating the effectiveness of health policies is crucial for ensuring that they achieve their intended goals and improve population health. This involves a systematic process of data collection, analysis, and impact assessment, allowing policymakers to understand the policy’s strengths, weaknesses, and areas for improvement.
The Process of Evaluating Health Policies
Evaluating health policies requires a structured approach to understand their impact on health outcomes and resource allocation. This involves:
- Defining the evaluation question:Clearly stating the purpose of the evaluation, including the specific policy being assessed and the desired outcomes.
- Identifying relevant data sources:Gathering data from various sources, such as government databases, surveys, health records, and existing research studies.
- Analyzing the data:Applying appropriate statistical methods to analyze the collected data and determine the policy’s impact on health outcomes, cost-effectiveness, and equity.
- Interpreting the findings:Drawing conclusions from the data analysis, considering the context and limitations of the evaluation.
- Disseminating the results:Sharing the findings with policymakers, stakeholders, and the public to inform decision-making and improve future policy development.
Key Indicators for Measuring Effectiveness
To assess the impact of health policies, specific indicators are used to measure key aspects of health and healthcare:
- Health outcomes:Mortality rates, morbidity rates, incidence and prevalence of diseases, life expectancy, quality-adjusted life years (QALYs), and self-reported health status.
- Healthcare utilization:Hospital admissions, outpatient visits, emergency department visits, and prescription drug use.
- Healthcare costs:Total healthcare spending, per capita healthcare spending, and cost-effectiveness of interventions.
- Access to healthcare:Insurance coverage, waiting times for appointments and procedures, and geographic access to healthcare services.
- Health equity:Disparities in health outcomes and healthcare access based on factors such as race, ethnicity, socioeconomic status, and geographic location.
Challenges in Evaluating Health Policies
Evaluating health policies can be complex due to several challenges:
- Data availability:Obtaining reliable and comprehensive data is crucial for accurate evaluation. However, data collection can be time-consuming, expensive, and subject to limitations in coverage and accuracy.
- Ethical considerations:Evaluations may involve sensitive personal information, requiring adherence to privacy regulations and informed consent from participants.
- Long-term impacts:Evaluating the long-term impacts of policies can be difficult, as it may take years to observe significant changes in health outcomes.
- Confounding factors:It can be challenging to isolate the effects of a specific policy from other factors that may influence health outcomes, such as socioeconomic conditions, environmental factors, and individual behaviors.
Examples of Successful and Unsuccessful Evaluations, Policies and health
- Successful evaluation:The National School Lunch Program (NSLP) in the United States has been evaluated extensively, demonstrating its effectiveness in improving the nutritional status of children. Studies have shown that participating in the NSLP is associated with lower rates of obesity, better dietary intake, and improved academic performance.
- Unsuccessful evaluation:The Affordable Care Act (ACA) in the United States, while successful in expanding insurance coverage, has faced challenges in achieving its goals of reducing healthcare costs and improving quality of care. Evaluations have shown mixed results, with some studies indicating cost increases and others showing improvements in quality measures.
Health Policy Advocacy and Engagement: Policies And Health

Advocacy plays a crucial role in shaping health policy decisions, ensuring that the needs and perspectives of diverse stakeholders are considered. By engaging in advocacy, individuals and organizations can influence policy development, implementation, and evaluation, ultimately contributing to healthier communities.
Strategies for Effective Health Policy Advocacy
Effective health policy advocacy involves a multi-faceted approach that combines strategic communication, relationship building, and community engagement. Here are some key strategies:
- Lobbying:Engaging with policymakers directly to advocate for specific policy changes. This can involve providing expert testimony, participating in legislative hearings, and meeting with elected officials to present evidence and arguments.
- Public Education:Raising awareness among the general public about health issues and the importance of specific policies. This can involve media campaigns, community outreach programs, and educational materials that inform and mobilize citizens.
- Community Organizing:Mobilizing community members to advocate for their own health needs. This can involve grassroots organizing, coalition building, and empowering communities to participate in policy decision-making.
Examples of Successful Health Policy Advocacy Campaigns
Numerous successful health policy advocacy campaigns have demonstrated the power of collective action in driving positive change.
- The Tobacco Control Act of 2009:This landmark legislation, passed in the United States, significantly restricted tobacco advertising and marketing, increased cigarette taxes, and funded public health programs to combat smoking. The campaign for this legislation involved a coalition of public health organizations, advocacy groups, and individuals who worked tirelessly to raise awareness, lobby policymakers, and mobilize public support.
- The Affordable Care Act (ACA):This comprehensive health reform law, enacted in 2010, expanded health insurance coverage to millions of Americans, provided subsidies to help individuals afford coverage, and implemented reforms to the health insurance market. The campaign for the ACA involved a broad coalition of advocacy groups, labor unions, consumer organizations, and individuals who advocated for the law’s passage and subsequent implementation.
Engaging Stakeholders in Health Policy Development and Implementation
Engaging stakeholders in the development and implementation of health policies is essential to ensure that policies are effective, equitable, and sustainable. Here’s a plan for fostering stakeholder engagement:
- Identify and map stakeholders:Identify all relevant stakeholders, including individuals, organizations, and communities that are affected by the policy. This can involve conducting stakeholder analysis, reviewing existing data, and consulting with experts.
- Establish communication channels:Create mechanisms for regular communication with stakeholders, such as meetings, workshops, online forums, and surveys. This ensures that stakeholders have access to information and can provide feedback.
- Facilitate collaborative decision-making:Involve stakeholders in the policy development process, providing opportunities for input and feedback. This can involve establishing advisory committees, conducting focus groups, and implementing participatory decision-making approaches.
- Monitor and evaluate policy implementation:Regularly monitor the implementation of the policy, collecting data on its effectiveness and impact on different stakeholders. This information can be used to make adjustments to the policy and ensure that it is meeting its objectives.
Last Word
As we navigate the intricate landscape of policies and health, it becomes clear that informed decision-making, effective advocacy, and continuous evaluation are vital for creating a healthier society. By understanding the multifaceted nature of this relationship, we can empower ourselves to advocate for policies that promote well-being, address health disparities, and ensure a brighter future for all.
FAQ Summary
What are some examples of policies that have negatively impacted health?
Policies that have negatively impacted health include budget cuts to public health programs, environmental regulations that prioritize economic growth over environmental protection, and policies that restrict access to healthy food in low-income communities.
How can I get involved in health policy advocacy?
There are many ways to get involved in health policy advocacy. You can contact your elected officials to express your views on health policy issues, join a health advocacy organization, or volunteer your time to educate your community about health policy.
What are the ethical considerations in evaluating health policies?
Ethical considerations in evaluating health policies include ensuring the privacy and confidentiality of data, protecting the rights of participants in research studies, and ensuring that evaluations are conducted in a fair and unbiased manner.