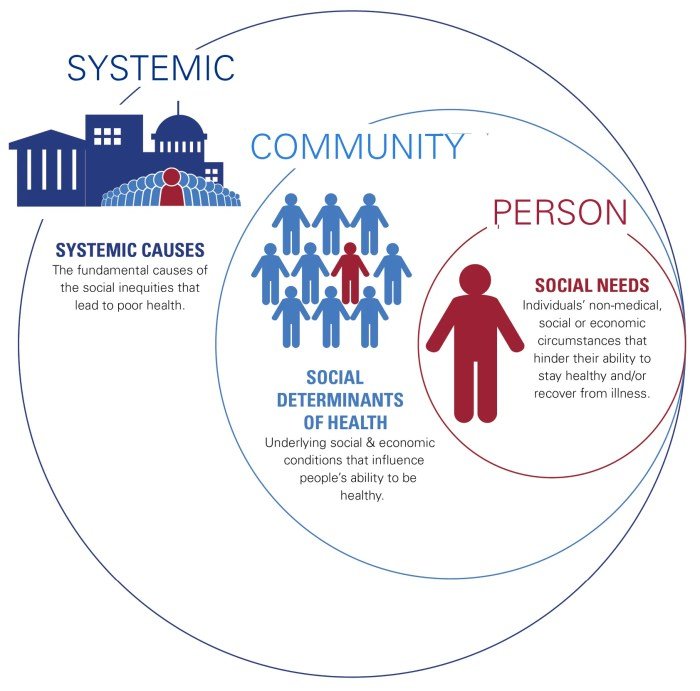
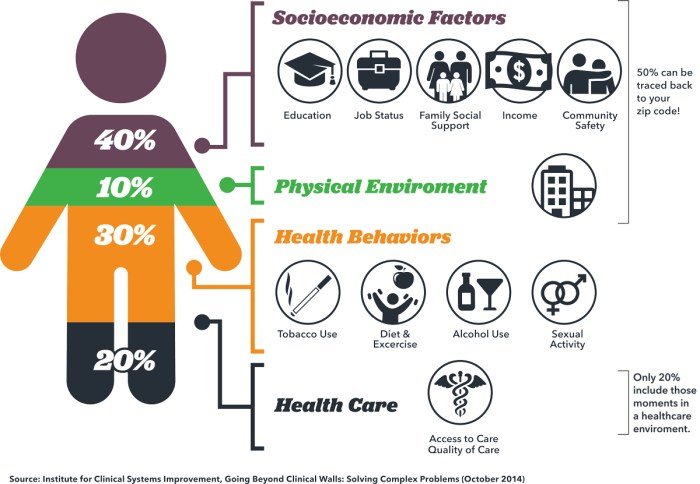
Social determinants in health (SDOH) are the non-medical factors that influence our health outcomes. These factors encompass a wide range of social, economic, and environmental conditions that shape our lives and well-being. From the neighborhoods we live in to the education we receive, SDOH play a crucial role in determining our health status.
Understanding these factors is essential for creating a healthier society and addressing health disparities.
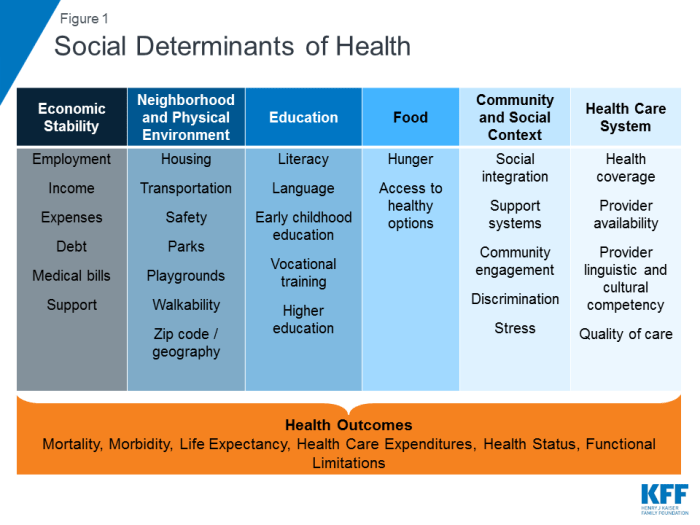
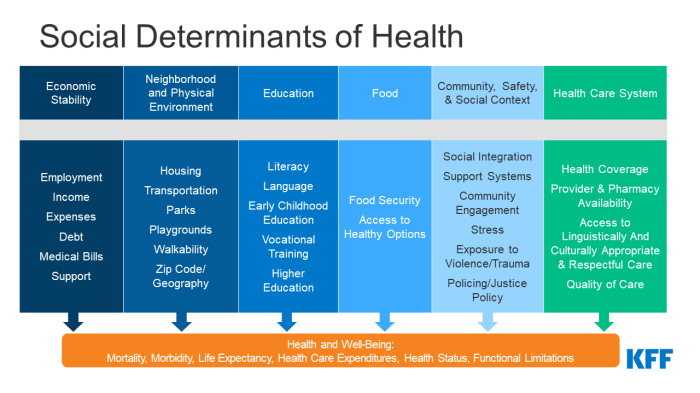
The historical context of SDOH reveals that health inequities have long been rooted in societal structures and systemic biases. These factors contribute to disparities in health outcomes, with certain groups experiencing poorer health than others. The key categories of SDOH include economic stability, education, social and community context, healthcare access, and neighborhood and built environment.
Each of these categories significantly influences health outcomes, creating a complex web of interconnected factors.
Introduction to Social Determinants of Health
Social determinants of health (SDOH) are the non-medical factors that influence an individual’s health status. They are the conditions in which people are born, grow, live, work, and age. These factors can have a significant impact on health outcomes, such as life expectancy, morbidity, and mortality.The understanding of SDOH has evolved over time.
Early public health initiatives focused primarily on infectious diseases and sanitation. As the understanding of health grew, the focus shifted to chronic diseases and lifestyle factors. In recent decades, there has been a growing recognition of the importance of SDOH in shaping health outcomes.
Key Categories of Social Determinants of Health
SDOH can be categorized into five key domains:
- Economic Stability: This includes factors such as income, employment, food security, and housing stability. For example, individuals with low incomes may have limited access to healthy food, safe housing, and healthcare. They may also be more likely to experience stress and other health problems related to poverty.
- Education: Education level is strongly associated with health outcomes. Individuals with higher levels of education tend to have better health outcomes, including lower rates of chronic diseases and higher life expectancy. This is likely due to a number of factors, including access to information, better employment opportunities, and healthier lifestyle choices.
- Social and Community Context: Social connections, community safety, and social support networks all play a role in health. For example, individuals with strong social support networks may be more likely to cope with stress and maintain healthy lifestyles. Conversely, individuals who experience social isolation or live in unsafe communities may be more vulnerable to health problems.
- Healthcare Access: This includes access to quality healthcare services, including preventative care, treatment, and medication. Individuals with limited access to healthcare may be more likely to experience health problems that go untreated or become more severe. They may also have difficulty accessing preventative care, which can help to prevent the development of chronic diseases.
- Neighborhood and Built Environment: This includes factors such as access to safe and affordable housing, transportation, and recreational opportunities. For example, individuals who live in neighborhoods with high crime rates or limited access to healthy food options may be more likely to experience health problems.
Conversely, individuals who live in neighborhoods with access to parks, green spaces, and other amenities may be more likely to engage in healthy behaviors.
Economic Stability: Social Determinants In Health
Economic stability plays a crucial role in shaping health outcomes, as it directly impacts individuals’ access to essential resources and opportunities. A lack of economic stability can create a cascade of negative effects on health, leading to health disparities and poorer overall well-being.
Income Inequality and Health Disparities, Social determinants in health
Income inequality, the uneven distribution of wealth within a society, has a profound impact on health disparities.
- Limited Access to Healthcare:Individuals with lower incomes often face barriers to accessing quality healthcare, including high healthcare costs, limited insurance coverage, and lack of access to specialized care. This can lead to delayed diagnoses, untreated conditions, and poorer health outcomes.
- Stress and Mental Health:Financial insecurity and the constant struggle to make ends meet can lead to chronic stress, anxiety, and depression. These mental health issues can negatively affect physical health, increasing the risk of heart disease, stroke, and other chronic conditions.
- Unhealthy Lifestyle Choices:Individuals with limited financial resources may be more likely to engage in unhealthy lifestyle choices, such as smoking, poor diet, and lack of physical activity, due to factors like limited access to healthy food options and safe spaces for exercise.
Studies have consistently shown a strong correlation between income inequality and health disparities. For example, a study published in the Journal of the American Medical Association found that individuals living in areas with higher income inequality had higher rates of mortality from heart disease, stroke, and cancer.
Education

Education plays a crucial role in shaping an individual’s health and well-being. A strong correlation exists between educational attainment and health status, indicating that higher levels of education are often associated with better health outcomes.
The Relationship Between Educational Attainment and Health Status
The relationship between education and health is multifaceted and complex. Individuals with higher levels of education tend to have:
- Improved health literacy:They possess a better understanding of health information, enabling them to make informed decisions about their health and well-being.
- Increased access to healthcare:Education often leads to better-paying jobs and health insurance coverage, improving access to preventive care and treatment.
- Healthier lifestyle choices:Educated individuals are more likely to engage in healthy behaviors such as regular exercise, balanced diets, and avoiding smoking and excessive alcohol consumption.
- Reduced exposure to risk factors:Education empowers individuals to make informed decisions that minimize their exposure to occupational hazards and other environmental risks.
The Impact of Early Childhood Development and Access to Quality Education on Health Outcomes
Early childhood development and access to quality education have a profound impact on health outcomes throughout life.
- Cognitive development:Early childhood education fosters cognitive development, enhancing problem-solving skills, critical thinking, and decision-making abilities, all of which contribute to better health outcomes.
- Social-emotional development:Quality education promotes social-emotional development, fostering empathy, self-regulation, and healthy relationships, all of which contribute to overall well-being.
- Health literacy:Early childhood education provides foundational knowledge about health and well-being, setting the stage for lifelong healthy habits and informed decision-making.
- Reduced health disparities:Access to quality education can help mitigate health disparities by providing equal opportunities for all children, regardless of their socioeconomic background.
The Role of Education in Promoting Health Literacy and Healthy Behaviors
Education plays a vital role in promoting health literacy and healthy behaviors.
- Health education programs:Schools and community organizations can implement health education programs to teach students about nutrition, physical activity, substance abuse prevention, and other health-related topics.
- Community outreach:Educational institutions can partner with community organizations to provide health education and resources to underserved populations.
- Promoting critical thinking:Education empowers individuals to critically evaluate health information from various sources, fostering informed decision-making about health and well-being.
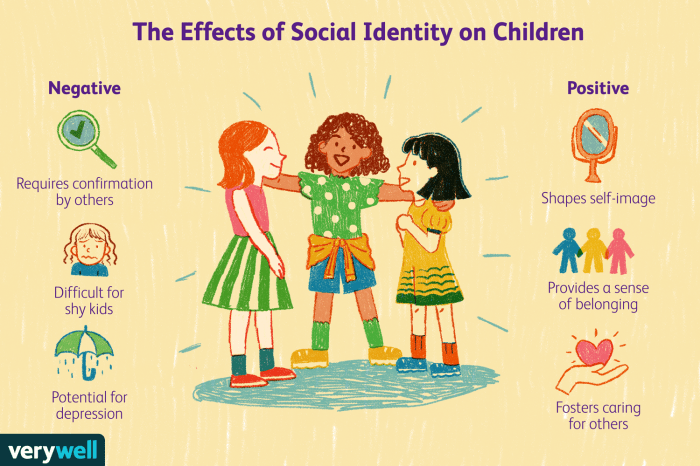
Social and Community Context
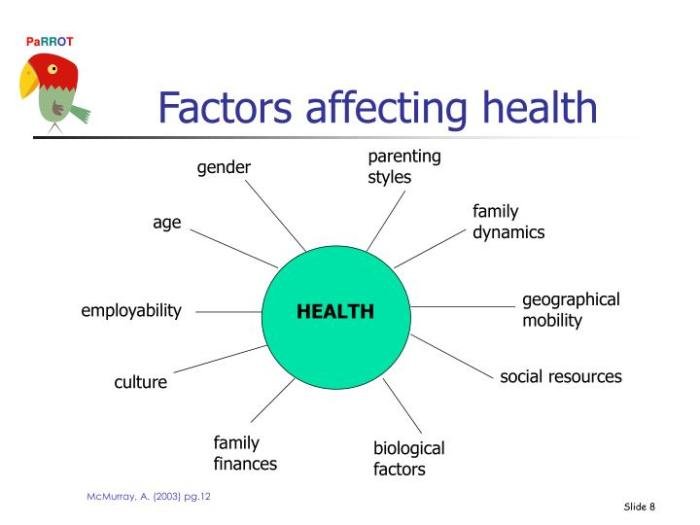
The social and community context in which people live has a profound impact on their health. This encompasses factors such as social isolation, discrimination, violence, community cohesion, and cultural norms, all of which play a significant role in shaping health outcomes.
Social Isolation, Discrimination, and Violence
Social isolation, discrimination, and violence are significant social determinants of health that can negatively affect individuals’ well-being. Social isolation, characterized by a lack of meaningful social connections, can lead to feelings of loneliness, depression, and anxiety, contributing to poor mental health.
Discrimination, based on factors such as race, ethnicity, gender, sexual orientation, or socioeconomic status, can lead to stress, anxiety, and depression, and can also limit access to resources and opportunities. Violence, including physical, sexual, and emotional abuse, can have devastating consequences for both physical and mental health.
Social determinants of health encompass a wide range of factors that influence our well-being, including access to safe and affordable housing, quality education, and opportunities for physical activity. Finding ways to incorporate exercise into our daily lives is crucial, and a great option is to explore health clubs near me with pool.
These facilities can provide a supportive environment for swimming, water aerobics, and other activities that benefit both physical and mental health, ultimately contributing to a healthier community.
Community Cohesion and Social Support Networks
Community cohesion, characterized by a sense of belonging, shared values, and mutual support, is essential for promoting health and well-being. Strong community cohesion fosters social support networks, which provide individuals with a sense of belonging, emotional support, and practical assistance.
These networks can help individuals cope with stress, navigate challenges, and access resources. Studies have shown that individuals with strong social support networks have better mental and physical health outcomes.
Cultural Norms and Beliefs
Cultural norms and beliefs play a significant role in shaping health behaviors and influencing health outcomes. Cultural norms can dictate dietary practices, health-seeking behaviors, and attitudes towards health and illness. For example, cultural beliefs about traditional medicine or the role of spirituality in health can influence individuals’ health choices.
Understanding cultural norms and beliefs is crucial for tailoring health interventions to meet the specific needs of different communities.
Healthcare Access
Access to healthcare is a fundamental social determinant of health, significantly influencing health outcomes. It encompasses the ability to obtain timely and appropriate medical care, including preventive services, treatment for acute and chronic conditions, and access to essential medications.
Impact of Insurance Coverage, Provider Availability, and Affordability on Health Disparities
Insurance coverage plays a pivotal role in accessing healthcare. Individuals with health insurance are more likely to receive preventive care, have regular check-ups, and manage chronic conditions effectively. However, disparities in insurance coverage persist, particularly among low-income individuals, minorities, and those with pre-existing conditions.
The lack of health insurance can lead to delayed or forgone care, resulting in poorer health outcomes and increased healthcare costs.
- Provider Availability: Access to healthcare is also influenced by the availability of healthcare providers, particularly in underserved areas. Rural communities often face a shortage of primary care physicians, specialists, and other healthcare professionals, limiting access to essential services. This shortage can lead to longer wait times for appointments, increased travel distances, and delayed or forgone care.
- Healthcare Affordability: The cost of healthcare is a significant barrier to access, particularly for low-income individuals and families. High deductibles, copayments, and out-of-pocket expenses can make healthcare unaffordable, leading to delayed or forgone care. This can exacerbate existing health disparities and create a cycle of poor health and financial hardship.
Role of Healthcare Quality and Patient-Centered Care in Addressing Health Inequities
Healthcare quality and patient-centered care are crucial in addressing health inequities. Providing high-quality care, tailored to individual needs and preferences, can improve health outcomes for all patients, regardless of their social determinants of health.
- Cultural Competency: Healthcare providers should be culturally competent, understanding and respecting the values, beliefs, and practices of diverse patient populations. This includes providing language interpretation services, incorporating culturally sensitive practices, and addressing health disparities related to race, ethnicity, gender, and sexual orientation.
- Patient-Centered Communication: Effective patient-centered communication is essential for building trust and ensuring that patients understand their health conditions, treatment options, and healthcare needs. This includes actively listening to patients, addressing their concerns, and involving them in decision-making about their care.
Neighborhood and Built Environment
The neighborhood and built environment play a crucial role in shaping health outcomes. Factors like safety, access to healthy food, quality housing, and environmental conditions significantly influence an individual’s overall well-being.
Impact of Neighborhood Factors on Health
The neighborhood environment can have a profound impact on health. Here are some key factors:
- Neighborhood Safety: Living in a neighborhood with high crime rates or violence can lead to stress, anxiety, and even physical injury. This can negatively affect mental and physical health. For example, residents in high-crime neighborhoods may experience elevated levels of cortisol, a stress hormone linked to various health problems.
- Access to Healthy Food: Limited access to affordable and nutritious food, often found in food deserts, contributes to poor dietary habits and chronic diseases like obesity, diabetes, and heart disease. Studies have shown that people living in food deserts have a higher prevalence of obesity and related health issues.
- Quality Housing: Inadequate housing conditions, such as overcrowding, poor ventilation, and exposure to lead paint, can lead to respiratory problems, asthma, and other health issues. For example, lead exposure in children can cause developmental delays and cognitive impairment.
Environmental Factors and Health Outcomes
Environmental factors within a neighborhood can significantly impact health.
- Air Pollution: Exposure to air pollutants from traffic, industrial emissions, and other sources can lead to respiratory problems, cardiovascular disease, and even cancer. For instance, studies have shown a correlation between increased air pollution levels and higher rates of asthma and lung cancer.
- Water Pollution: Contaminated water sources can lead to waterborne illnesses and other health problems. For example, exposure to lead in drinking water can cause developmental delays and cognitive impairment in children.
Role of Transportation Infrastructure and Community Design
The design of transportation infrastructure and community spaces can influence physical activity levels and overall health.
- Walkability and Bikeability: Neighborhoods with sidewalks, bike lanes, and parks encourage physical activity and reduce reliance on cars. This can lead to lower rates of obesity, heart disease, and other chronic diseases. For example, studies have shown that people living in walkable neighborhoods have lower body mass indexes and are more likely to engage in regular physical activity.
- Community Design: Community design that prioritizes green spaces, parks, and recreational facilities promotes physical activity and social interaction, contributing to better mental and physical health. For instance, communities with parks and green spaces have been shown to have lower rates of depression and anxiety.
Social determinants of health, like socioeconomic status and access to healthcare, play a crucial role in shaping health outcomes. Understanding these factors is vital for the division of health sciences as it helps researchers and practitioners develop effective interventions to address health disparities and promote health equity.
Addressing Social Determinants of Health
Addressing social determinants of health (SDOH) is crucial for achieving health equity and improving overall well-being. This involves implementing strategies that mitigate the impact of these factors on health outcomes, recognizing that individuals’ health is shaped by a complex interplay of social, economic, and environmental factors.
Public Policy Interventions
Public policy plays a vital role in addressing health inequities by creating a supportive environment that promotes health and well-being for all. Effective policies can address the root causes of health disparities and create a level playing field for individuals and communities.
- Expanding Access to Affordable Housing:Housing instability is a significant SDOH, contributing to poor health outcomes. Policies aimed at increasing affordable housing options, such as rent control measures and subsidies, can help alleviate housing insecurity and improve health. For instance, the “Housing First” model has been shown to effectively address homelessness and improve health outcomes for individuals experiencing homelessness.
- Investing in Quality Education:Education is a powerful tool for improving health outcomes. Policies that promote access to quality education, from early childhood to higher education, can empower individuals with the knowledge, skills, and resources needed to lead healthy lives. Studies have shown a strong correlation between education levels and health outcomes, with higher levels of education associated with better health and longer lifespans.
- Promoting Employment Opportunities:Economic stability is a fundamental SDOH. Policies that create a robust job market, provide living wages, and support workforce development can help individuals achieve financial security and improve their health. The creation of job training programs and initiatives that promote job growth in underserved communities can address unemployment and improve economic well-being.
Social determinants of health encompass a wide range of factors that influence our well-being, from access to quality healthcare to the neighborhoods we live in. These factors even extend to how we perceive and define beauty , which can be influenced by cultural norms and societal expectations.
Ultimately, understanding these social determinants is crucial for creating a healthier and more equitable society for all.
Community-Based Interventions
Community-based interventions are essential for addressing the unique needs and challenges of local populations. These interventions can leverage the strengths and resources of communities to promote health and well-being.
- Community Health Centers:Community health centers provide comprehensive primary care services to underserved populations, often located in areas with limited access to healthcare. They offer a range of services, including preventive care, chronic disease management, and mental health support. For example, the Federally Qualified Health Center (FQHC) program in the United States provides funding and support to community health centers, enabling them to serve millions of low-income and uninsured individuals.
- Community Gardens:Community gardens provide opportunities for residents to grow fresh fruits and vegetables, promoting healthy eating habits and access to nutritious food. They also foster social connections and community engagement, contributing to overall well-being. For example, the “GrowNYC” program in New York City has established over 500 community gardens across the city, providing access to fresh produce and promoting healthy lifestyles.
- Social Support Networks:Strong social support networks are crucial for mental and physical health. Community-based interventions can foster social connections by organizing community events, creating safe spaces for social interaction, and providing support groups for individuals facing specific challenges. For example, the “Meals on Wheels” program provides home-delivered meals to seniors and individuals with disabilities, promoting social interaction and reducing social isolation.
Individual-Level Actions
While systemic changes are essential, individuals can also take proactive steps to address the impact of SDOH on their health.
- Advocacy and Community Engagement:Individuals can raise awareness about SDOH and advocate for policies that promote health equity. They can participate in community organizations, engage in public dialogue, and contact elected officials to voice their concerns and support initiatives that address SDOH.
- Healthy Lifestyle Choices:Individuals can make healthy lifestyle choices, such as eating a balanced diet, engaging in regular physical activity, and managing stress, to improve their overall health and well-being. However, it is important to recognize that these choices can be limited by SDOH, such as access to healthy food options, safe places to exercise, and affordable healthcare.
- Seeking Support and Resources:Individuals facing challenges related to SDOH can seek support from community organizations, healthcare providers, and social services. They can access resources such as food banks, housing assistance programs, and mental health services to address their needs and improve their health outcomes.
Implications for Healthcare and Public Health
Understanding the social determinants of health (SDOH) is crucial for healthcare providers and public health professionals. These factors have a profound impact on health outcomes, and addressing them is essential for improving population health.
Addressing SDOH in Healthcare Systems
A comprehensive approach to addressing SDOH in healthcare systems is vital for achieving health equity. This involves integrating SDOH considerations into all aspects of healthcare delivery, from patient intake to treatment planning and discharge.
- Screening for SDOH:Healthcare providers should routinely screen patients for SDOH factors, such as income, housing, food security, and transportation. This information can help identify patients who are at risk for health disparities and provide them with tailored support.
- Connecting Patients to Resources:Healthcare providers should connect patients to community resources that can address their SDOH needs. This could include food banks, housing assistance programs, and transportation services.
- Advocating for Policy Changes:Healthcare providers should advocate for policy changes that address the root causes of SDOH. This could include policies that increase access to affordable housing, education, and employment.
Addressing SDOH in Public Health Systems
Public health professionals play a critical role in addressing SDOH by promoting policies and programs that create healthy environments and reduce health disparities.
- Community Health Assessments:Public health agencies should conduct community health assessments to identify SDOH factors that are contributing to health disparities in their communities.
- Health Education and Outreach:Public health professionals should provide health education and outreach programs that address SDOH factors and empower individuals to make healthy choices.
- Collaboration with Community Partners:Public health professionals should collaborate with community partners, such as schools, businesses, and faith-based organizations, to address SDOH factors.
Role of Data and Research
Data and research are essential for informing interventions and policies related to SDOH.
- Collecting and Analyzing Data:Public health agencies and healthcare organizations should collect and analyze data on SDOH factors to identify trends and disparities.
- Evaluating Interventions:Research is needed to evaluate the effectiveness of interventions aimed at addressing SDOH.
- Developing Evidence-Based Policies:Data and research can inform the development of evidence-based policies that address SDOH.
Ending Remarks

By recognizing the impact of SDOH, we can implement targeted interventions and policies that address the root causes of health disparities. A comprehensive approach that addresses SDOH requires collaboration between healthcare providers, public health professionals, community organizations, and policymakers.
This collaborative effort is essential for creating a healthier and more equitable society for all.
FAQ Summary
What are some examples of social determinants of health?
Examples of SDOH include income level, education attainment, access to healthcare, neighborhood safety, and exposure to environmental hazards.
How do social determinants of health affect health outcomes?
SDOH can influence health outcomes by impacting factors such as stress levels, access to healthy food, exposure to violence, and opportunities for physical activity.
What can be done to address social determinants of health?
Addressing SDOH requires a multi-pronged approach that includes policy changes, community-based interventions, and individual-level actions. This could involve increasing access to affordable housing, improving educational opportunities, and promoting healthy food options in low-income communities.