Social determinants of health defined are the non-medical factors that influence an individual’s health status. These factors are often overlooked but play a crucial role in shaping health outcomes, often contributing to health disparities and inequalities.
Imagine a community where residents lack access to affordable housing, nutritious food, or quality education. These social factors create a ripple effect, leading to higher rates of chronic diseases, mental health issues, and overall poorer health outcomes. Understanding these social determinants is vital for developing effective health interventions and achieving health equity.
Defining Social Determinants of Health

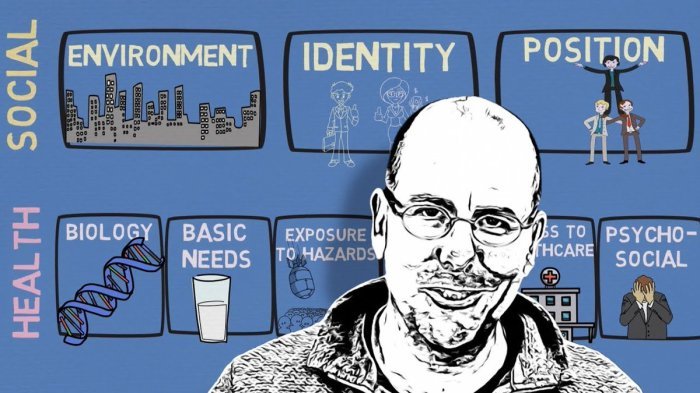
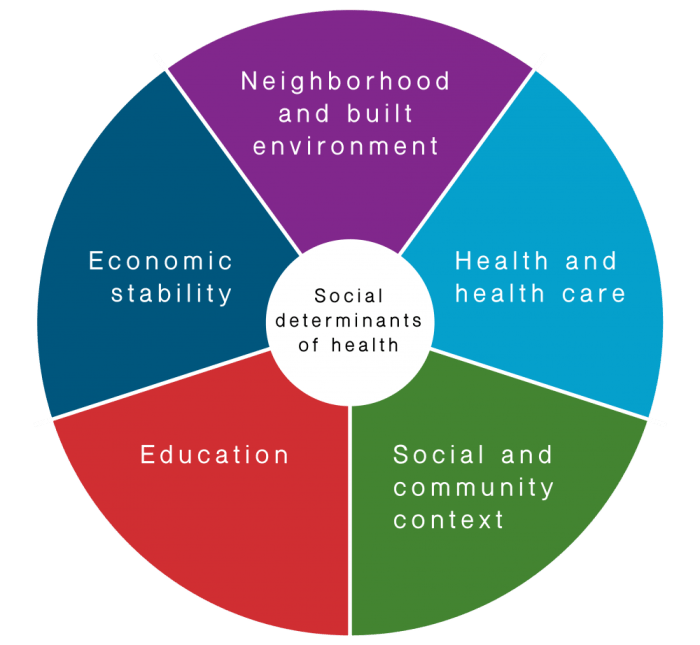
Understanding the factors that influence a person’s health goes beyond just medical care. Social determinants of health (SDOH) encompass the broader societal and environmental conditions that shape health outcomes. They are the non-medical factors that can significantly impact an individual’s health and well-being.
Social determinants of health, those factors that influence an individual’s health outside of their medical care, are increasingly recognized as crucial to overall well-being. Companies like Agilon Health stock , which focuses on value-based care for Medicare Advantage patients, are beginning to incorporate these factors into their models, acknowledging that health is a complex interplay of social, economic, and environmental factors.
Social Determinants of Health: A Comprehensive Definition
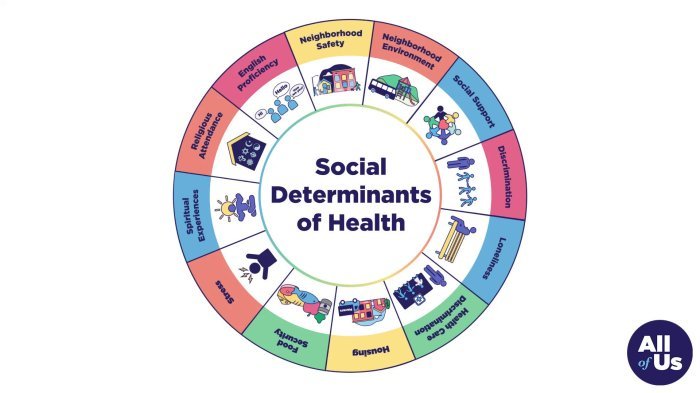
Social determinants of health (SDOH) are the conditions in which people are born, grow, live, work, and age. They are the factors that influence a wide range of health outcomes, including life expectancy, morbidity, and overall well-being.
Key Factors Contributing to Social Determinants of Health
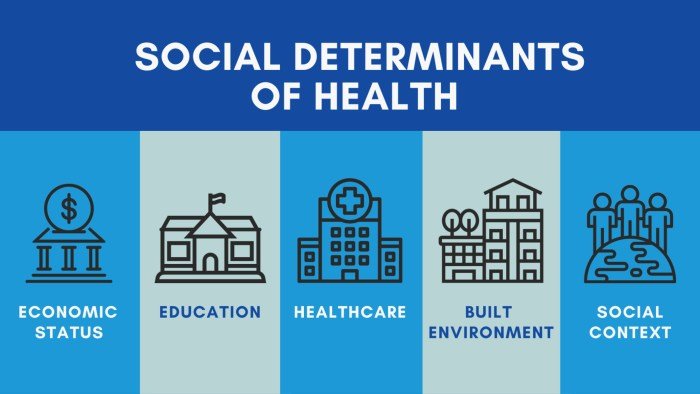
A wide range of factors contribute to SDOH, and these factors can interact in complex ways. Here are some key examples:
- Socioeconomic Status:Income, wealth, and occupation can significantly influence access to resources, such as healthy food, safe housing, and quality education, all of which impact health. For example, individuals living in poverty may face challenges in accessing nutritious food, which can lead to dietary deficiencies and health problems.
Social determinants of health encompass the social, economic, and environmental factors that influence our well-being. These factors can range from access to quality healthcare and education to the presence of safe and affordable housing. Even seemingly unrelated things, like the availability of beauty products at places like sephora rare beauty , can contribute to an individual’s sense of self-worth and ultimately, their overall health.
Understanding these interconnected factors is crucial for creating a society that prioritizes health equity for all.
- Education:Educational attainment is strongly linked to health outcomes. Higher levels of education are associated with better health literacy, access to information, and employment opportunities, leading to improved health choices and overall well-being.
- Access to Healthcare:Having affordable and readily available healthcare services is crucial for maintaining good health. Barriers to access, such as high healthcare costs, limited insurance coverage, and geographical distance to healthcare facilities, can significantly impact health outcomes.
- Environmental Conditions:The physical environment in which people live can influence their health. Factors like air and water quality, access to green spaces, and exposure to environmental hazards can impact health outcomes. For instance, living in areas with high levels of air pollution can contribute to respiratory problems and other health issues.
Impact of SDOH on Health Outcomes
Social determinants of health (SDOH) are the non-medical factors that influence health outcomes. These factors are deeply rooted in the social fabric of society and can significantly impact health disparities and inequalities. They are the conditions in which people are born, grow, live, work, and age.
Understanding the impact of SDOH on health outcomes is crucial for developing effective health interventions and promoting health equity.
Influence of SDOH on Health Outcomes
SDOH play a critical role in shaping health outcomes across various dimensions, including morbidity, mortality, and overall well-being. They can either positively or negatively impact health, depending on their influence.
- Morbidity:SDOH can significantly influence the prevalence of chronic diseases, infectious diseases, and mental health conditions. For instance, limited access to healthy food and safe housing can increase the risk of obesity, diabetes, and cardiovascular disease. Similarly, exposure to environmental hazards, such as air pollution, can contribute to respiratory illnesses.
- Mortality:SDOH factors can also impact mortality rates. For example, individuals living in poverty or with limited access to healthcare may have higher mortality rates due to delayed diagnoses, inadequate treatment, and preventable health complications.
- Overall Well-being:SDOH contribute to overall well-being, encompassing physical, mental, and social health. Factors like education, employment, and social support systems can positively impact well-being by promoting healthy habits, reducing stress, and fostering a sense of belonging.
Examples of SDOH Factors and Health Disparities
Specific SDOH factors can lead to health disparities and inequalities across different population groups. For instance:
- Education:Individuals with lower levels of education may experience higher rates of chronic diseases and premature mortality. This can be attributed to factors such as lower income, limited access to healthcare, and unhealthy lifestyle choices.
- Income:Low-income individuals often face significant health challenges, including limited access to nutritious food, safe housing, and healthcare. These factors can contribute to increased risk of chronic diseases and reduced life expectancy.
- Neighborhood and Built Environment:The physical environment where people live can have a profound impact on health. For example, neighborhoods with limited access to parks, green spaces, and healthy food options can contribute to obesity and other health problems.
Relationship between SDOH and Chronic Diseases
SDOH play a significant role in the development and progression of chronic diseases. For example:
- Heart Disease:Factors such as poverty, lack of access to healthcare, and exposure to air pollution can increase the risk of heart disease.
- Diabetes:Limited access to healthy food, physical inactivity, and lack of healthcare can contribute to the development and management of diabetes.
- Cancer:Environmental factors, such as exposure to carcinogens in the workplace or neighborhood, can increase the risk of cancer.
Relationship between SDOH and Mental Health Issues
SDOH factors can significantly impact mental health outcomes. For instance:
- Stress:Poverty, unemployment, and exposure to violence can contribute to chronic stress, which can lead to anxiety, depression, and other mental health problems.
- Social Isolation:Lack of social support and connections can increase the risk of loneliness and depression.
- Discrimination:Discrimination based on race, ethnicity, gender, or sexual orientation can contribute to mental health issues, including stress, anxiety, and depression.
Relationship between SDOH and Infectious Diseases
SDOH can influence the spread and severity of infectious diseases. For example:
- Access to Healthcare:Limited access to healthcare can delay diagnosis and treatment, leading to increased transmission of infectious diseases.
- Housing Conditions:Overcrowded and unsanitary housing conditions can promote the spread of infectious diseases, such as tuberculosis and influenza.
- Environmental Factors:Exposure to contaminated water or air can increase the risk of contracting infectious diseases.
Addressing SDOH in Healthcare
The recognition of social determinants of health (SDOH) as critical drivers of health outcomes has led to a growing emphasis on incorporating SDOH considerations into healthcare systems and practices. This shift requires a comprehensive approach that goes beyond traditional clinical care and addresses the social, economic, and environmental factors that influence health.
Framework for Incorporating SDOH Considerations
A robust framework for integrating SDOH considerations into healthcare systems should encompass several key elements:
- Data Collection and Screening:Healthcare providers should routinely collect data on patients’ SDOH factors, such as socioeconomic status, housing conditions, food security, and access to transportation. This information can be gathered through standardized questionnaires, patient interviews, or community health assessments.
- Risk Assessment and Prioritization:Once data is collected, healthcare systems can develop risk assessment tools to identify individuals at higher risk for adverse health outcomes due to SDOH challenges. This allows for targeted interventions and resource allocation.
- Interdisciplinary Collaboration:Addressing SDOH requires collaboration among healthcare professionals, community organizations, and social service providers. This interdisciplinary approach ensures a holistic understanding of patients’ needs and facilitates the coordination of services.
- Community Partnerships:Healthcare systems should actively engage with community organizations, local leaders, and residents to understand local SDOH challenges and develop tailored solutions. This fosters trust and builds community capacity to address health disparities.
- Policy Advocacy:Healthcare organizations can play a crucial role in advocating for policies that address SDOH at the local, state, and national levels. This includes supporting initiatives that promote affordable housing, living wages, and access to healthy food.
Strategies and Interventions
Various strategies and interventions can effectively address SDOH challenges and improve health outcomes.
- Housing Stability Programs:Programs that provide housing assistance, eviction prevention services, and rental subsidies can reduce housing insecurity and improve health outcomes. For example, the Housing First program prioritizes providing permanent housing for individuals experiencing homelessness, which has been shown to improve their health and well-being.
- Food Security Initiatives:Addressing food insecurity through programs like food banks, community gardens, and nutrition education can enhance access to nutritious food and reduce the risk of chronic diseases. The Supplemental Nutrition Assistance Program (SNAP) provides financial assistance to low-income families for food purchases, helping them meet their nutritional needs.
- Transportation Assistance:Providing transportation assistance, such as ride-sharing programs or public transportation vouchers, can improve access to healthcare appointments, employment opportunities, and essential services. This can be particularly beneficial for individuals in rural areas or those with limited mobility.
- Financial Counseling and Support:Financial counseling and support programs can help individuals manage their finances, reduce debt, and improve their financial stability. This can alleviate stress and improve overall health outcomes.
- Social Connection and Support:Promoting social connection and support through community centers, senior centers, and social support groups can mitigate the negative impacts of social isolation and loneliness, which are associated with poorer health outcomes.
Role of Community Partnerships and Interdisciplinary Collaboration
Community partnerships and interdisciplinary collaboration are essential for effectively addressing SDOH.
- Community Health Workers:Community health workers, often members of the communities they serve, can act as trusted intermediaries between healthcare providers and patients, facilitating access to services and addressing cultural and linguistic barriers. They can also provide education and support related to SDOH factors.
- Community-Based Organizations:Partnering with community-based organizations, such as faith-based groups, social service agencies, and neighborhood associations, allows healthcare systems to leverage their expertise and resources to address SDOH challenges within specific communities.
- Interdisciplinary Teams:Interdisciplinary teams that include physicians, nurses, social workers, community health workers, and other professionals can provide a holistic approach to patient care, addressing both clinical and social needs.
- Data Sharing and Coordination:Effective collaboration requires the sharing of data and information between healthcare providers, community organizations, and social service providers. This ensures that individuals receive the appropriate support and services across different sectors.
Policy and Advocacy for SDOH
Public policies play a crucial role in shaping the social determinants of health (SDOH) and ultimately influencing health outcomes. Recognizing the impact of these policies is essential to identify areas for improvement and advocate for changes that promote health equity.
Impact of Public Policies on SDOH
Public policies can either contribute to or exacerbate health disparities. For instance, policies related to housing, education, employment, and access to healthcare directly influence SDOH factors.
Social determinants of health encompass the factors that influence an individual’s health outcomes, including socioeconomic status, education, and access to healthy food. The availability of nutritious food, like those found in Chinese health food traditions, can significantly impact health outcomes.
Therefore, addressing social determinants of health requires a holistic approach that considers the diverse factors contributing to well-being.
- Housing policies:Affordable housing policies, zoning regulations, and eviction protections directly impact housing stability and affordability, which in turn affect health outcomes. For example, lack of access to safe and affordable housing can lead to increased stress, exposure to environmental hazards, and limited access to healthcare.
- Education policies:Policies that promote early childhood education, provide access to quality education, and support student success can positively influence health outcomes by improving cognitive development, increasing earning potential, and reducing health risks. Conversely, inadequate education funding, limited access to early childhood education, and high school dropout rates can contribute to poor health outcomes.
- Employment policies:Minimum wage laws, worker protections, and access to paid leave can impact employment stability, income security, and work-related stress. Policies that ensure fair wages, safe working conditions, and access to paid leave can promote better health outcomes. Conversely, policies that result in low wages, job insecurity, and lack of work-life balance can negatively impact health.
- Healthcare policies:Policies related to access to healthcare, coverage, and affordability directly influence health outcomes. Expanding access to healthcare through programs like Medicaid, Medicare, and affordable insurance options can improve health outcomes. Conversely, policies that restrict access to healthcare, limit coverage, or increase costs can worsen health disparities.
Policy Recommendations to Address SDOH, Social determinants of health defined
Recognizing the impact of public policies on SDOH, it is essential to advocate for policies that promote health equity.
- Expand access to affordable housing:Policies should prioritize the development of affordable housing options, strengthen tenant protections, and prevent displacement due to gentrification.
- Invest in early childhood education:Policies should ensure access to quality early childhood education for all children, regardless of socioeconomic background.
- Promote fair labor practices:Policies should ensure living wages, safe working conditions, paid leave, and access to affordable childcare for working families.
- Expand access to healthcare:Policies should expand access to affordable healthcare through programs like Medicaid and Medicare, reduce out-of-pocket costs, and address healthcare disparities.
- Address environmental health risks:Policies should promote clean air and water, reduce exposure to environmental toxins, and invest in sustainable infrastructure.
Importance of Advocacy Efforts
Advocacy efforts are crucial in raising awareness about SDOH and promoting policy changes that address health disparities.
- Educate policymakers and the public:Advocacy organizations can educate policymakers and the public about the impact of SDOH on health outcomes and the need for policy changes.
- Build coalitions and partnerships:Advocacy groups can build coalitions with other organizations and community leaders to advocate for policy changes.
- Promote community engagement:Advocacy efforts should encourage community engagement and empower communities to advocate for their own health needs.
- Monitor policy implementation:Advocacy organizations can monitor the implementation of policies and hold policymakers accountable for their commitments.
Examples of SDOH in Action

Social determinants of health (SDOH) are the conditions in which people are born, grow, live, work, and age. These factors can have a profound impact on health outcomes, often influencing health disparities and inequalities. This section will delve into real-world examples that showcase how SDOH factors influence health outcomes in specific populations or communities.
Examples of SDOH Impacting Health Outcomes
The impact of SDOH on health outcomes can be observed across various communities and populations. Below are some examples that highlight the intricate interplay between SDOH factors and health:
| SDOH Factor | Population/Community | Health Outcome | Intervention |
|---|---|---|---|
| Education | Low-income neighborhoods | Higher rates of chronic diseases, such as diabetes and heart disease | Expanding access to quality education, providing health literacy programs, and promoting community-based health education initiatives. |
| Economic Stability | Individuals experiencing homelessness | Increased risk of infectious diseases, mental health issues, and substance abuse | Providing affordable housing options, job training programs, and financial assistance. |
| Neighborhood and Built Environment | Communities with limited access to green spaces | Higher rates of obesity, physical inactivity, and respiratory problems | Creating walkable communities, promoting access to parks and recreational facilities, and implementing urban greening projects. |
| Social and Community Context | Immigrant communities | Language barriers, cultural differences, and lack of social support can lead to disparities in healthcare access and utilization | Providing culturally competent healthcare services, promoting language interpretation services, and fostering community engagement. |
| Healthcare Access and Quality | Rural communities | Limited access to specialized healthcare services, longer wait times, and lower quality of care | Expanding telehealth services, increasing the number of healthcare providers in rural areas, and investing in infrastructure to improve healthcare access. |
The Future of SDOH: Social Determinants Of Health Defined
The field of social determinants of health (SDOH) is rapidly evolving, driven by a growing understanding of their profound impact on health outcomes and a commitment to achieving health equity. As we look ahead, several emerging trends and challenges will shape the future of SDOH, alongside exciting opportunities for innovation and progress.
Emerging Trends and Challenges
The future of SDOH is marked by both exciting opportunities and significant challenges. Recognizing and addressing these aspects is crucial for effective progress.
- Increased Data Availability and Analytics: Advances in data collection, analysis, and artificial intelligence (AI) are providing unprecedented insights into the complex interplay between SDOH and health outcomes. This data-driven approach allows for more targeted interventions and policy decisions. For example, analyzing large datasets can help identify neighborhoods with high rates of chronic diseases, enabling the development of community-based programs to address underlying SDOH factors.
- Growing Focus on Health Equity: The movement towards health equity is gaining momentum, demanding a more equitable distribution of resources and opportunities to improve health for all. This focus will necessitate a systemic approach to address SDOH, dismantling social and economic barriers that perpetuate health disparities.
- Intersectionality and Complexities: Recognizing the interconnectedness of SDOH factors is crucial. Addressing one factor in isolation may not be effective. For instance, improving access to healthy food may not be sufficient if individuals lack safe and affordable housing or face discrimination in employment opportunities.
- Integration of SDOH into Healthcare Systems: The need for healthcare systems to comprehensively address SDOH is becoming increasingly evident. This requires integrating SDOH screening and interventions into routine clinical care, fostering collaboration with community organizations, and addressing social needs alongside medical needs.
- Sustainability and Long-Term Impact: Achieving lasting improvements in health equity requires sustainable solutions that address the root causes of SDOH. This involves investing in community development, promoting economic opportunities, and strengthening social safety nets.
Impact of Technology and Innovation
Technological advancements offer promising opportunities to address SDOH and improve health equity.
- Telehealth and Remote Monitoring: Telehealth technologies enable access to healthcare services for individuals in underserved communities, bridging geographical barriers and improving access to preventive care and chronic disease management.
- Data-Driven Interventions: AI-powered analytics can help identify individuals at risk of health problems due to SDOH factors, enabling targeted interventions and resource allocation.
- Community-Based Solutions: Mobile apps and online platforms can empower communities to connect, share resources, and advocate for change. For example, apps can provide information about local food banks, transportation options, and community health programs.
- Precision Public Health: Leveraging data and technology to tailor interventions to specific populations and communities based on their unique SDOH profiles can optimize resource allocation and improve health outcomes.
Vision for the Future
Imagine a future where SDOH are effectively addressed, leading to a healthier and more equitable society.
A future where everyone has the opportunity to thrive, regardless of their zip code, race, ethnicity, or socioeconomic status.
- Universal Access to Quality Healthcare: Every individual has access to comprehensive, affordable, and culturally competent healthcare services, regardless of their ability to pay.
- Empowered Communities: Communities are actively engaged in shaping their health and well-being, with access to resources and opportunities to address SDOH factors.
- Data-Driven Equity: Data is used to identify and address health disparities, ensuring that resources are allocated equitably and interventions are tailored to specific needs.
- Sustainable Solutions: Long-term investments in community development, economic opportunities, and social safety nets create a foundation for lasting improvements in health equity.
Last Point
By addressing the social determinants of health, we can create a society where everyone has the opportunity to live a healthy life. This requires a collaborative effort involving healthcare providers, policymakers, community organizations, and individuals. Together, we can break down the barriers that prevent people from achieving their full health potential and build a healthier future for all.
FAQ Overview
What are some examples of social determinants of health?
Examples include socioeconomic status, education level, access to healthcare, neighborhood safety, and environmental conditions.
How can I get involved in addressing social determinants of health?
You can volunteer with community organizations, advocate for policy changes, and educate yourself and others about the importance of social determinants of health.
What are some resources available for addressing social determinants of health?
The Centers for Disease Control and Prevention (CDC), the World Health Organization (WHO), and numerous non-profit organizations offer resources and information on social determinants of health.